Cracking the code used by human cells to exchange messages that affect health
Researchers discover how some microRNA gets picked to travel inside tiny sacs to other organs and regulate metabolism at a distance. The finding could improve early cancer diagnosis and help treat diabetes and high cholesterol
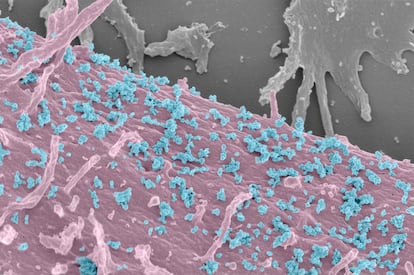
Human beings’ biggest conversations take place within their own bodies. Individuals are made up of around 30 trillion cells: neurons, red blood cells, fat cells... For many decades, the scientific community believed that each one of these cells disposed of its waste by secreting minuscule sacs measuring around 100 millionths of a millimeter, but this was a major mistake. Fifteen years ago, a team led by the Swedish scientist Jan Lötvall discovered that those tiny vesicles, called exosomes, were not really sacs filled with waste but packets with genetic information that traveled across the body. It was a remote communication system between human cells. Now, a team from Harvard University led by the Spanish biologist Rubén García and US doctor Ronald Kahn has shed new light on the inner workings of this massive internal conversation.
Exosomes are at the center of an ongoing medical revolution. Healthy cells send all kinds of messages through these vesicles, but so do diseased cells. Malignant cancer cells, for instance, use this communication channel to prepare their spread to other organs through metastasis. Intercepting and decoding these messages would allow doctors to diagnose disease much sooner than they can now, based on simple blood or urine samples. But the problem is that we’re not talking about listening in on a conversation between two cells. This is a cacophony of 30 trillion cells, each of which secretes thousands of vesicles each day.
Rubén García, a 35-year-old biologist who was raised in Alcorcón, near Madrid, describes the system as a kind of microscopic post office where cells send marked packages. “It is possible that some vesicles from one cell are carrying a specific load that’s going to the liver, while other vesicles are delivering to a muscle cell and carrying completely different content,” he said. “That’s the current hypothesis, but there is no proof yet.”
García’s team studied cells from five tissues – liver, skeletal muscle, blood vessels, white fat and brown fat (two types of adipose tissue in mammals) and found that each type sends out packages with characteristic content. The messages are written in the same language: microRNA, tiny molecules that are similar to words made up of around 20 chemical letters. Scientists at Harvard have discovered specific syllables that determine whether these words have to exit the cell or remain inside it. “Each type of cell has its own codes,” said García.
The new results suggest that it is possible to intercept a cellular message in a blood test and find out what type of cell sent it, says the Peruvian biologist Morayma Temoche. “It could help detect early-stage cancer and determine what tissue has been compromised,” said this researcher, who did not participate in the study. Temoche, who works for the US biotech company Metagenomi, earned her Ph.D. two years ago at the laboratory of Randy Schekman, winner of the 2013 Nobel Prize in medicine for his discoveries of the machinery regulating vesicle traffic. MicroRNA has already been used in recent years as biomarkers for the diagnosis of certain tumors, but their usefulness has been dragged down by the complexity and errors that still plague the technology.
Temoche said that the sequences of letters detected in microRNA “work like a ZIP code” that determines whether the message gets sent out or remains inside the cell. If those codes can be generalized, said the biologist, the discovery would be “a turning point” because it would allow scientists to prepare packages with therapeutic messages by adding the necessary sequence of letters.
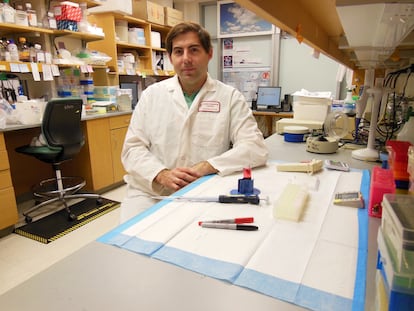
Rubén García compared the vesicle system with “a large distribution company like Amazon.” In this example, the products for sale would be the microRNA molecules, which would be packed into the exosomes and contain a “barcode” to identify the route they need to take. “One of the biggest challenges for the coming years is discovering which brands, which address labels are being carried by those exosomes to transport their contents to this organ and not that one,” said García, who is planning to join the National Biotechnology Center in Madrid this year to try to find out.
García is still working at the Joslin Diabetes Center, a teaching and research affiliate of the Harvard Medical School in Boston. This lab, which is headed by Ronald Kahn, showed in 2017 that fat cells release a large number of vesicles with microRNA that circulate in the blood and can regulate the metabolism of glucose in the liver. In a new study published on December 22 in the journal Nature, García and his colleagues showed through human cell cultures that it is possible to control the liver’s handling of sugars by genetically modifying the barcode of microRNA in fat.
The Harvard team is now exploring potential treatments against diabetes and other metabolic disorders. “With these new findings, we could genetically manipulate a microRNA in the easily accessible subcutaneous fat to target improving metabolism in the liver, which is much more difficult for direct gene therapy,” said the researchers in a statement. “And if something went wrong, we could always take out the fat, whereas you can’t take out the liver.”
They could enhance the effects over time, so that medication would need to be injected less frequentlyRubén García, Joslin Diabetes Center of Harvard Medical School
García also believes that their research can build the foundation for new strategies. “This system can be manipulated to make the desired microRNA go to the vesicles in a larger or smaller amount, and use this means of communication to change the genetic expression of the target cells and presumably their behavior as well,” he explained. “You could take tissue from a patient, modify it so that the microRNA you want gets loaded up in the vesicles, then put it back in the patient as a constant source of microRNA that gets sent inside vesicles to the necessary organs, say to those affected by a tumor or another disease.”
García underscored the pioneering work in this field of Francisco Sánchez Madrid, María Mittelbrunn and Carolina Villarroya, three scientists at Spain’s National Cardiovascular Research Center (CNIC) who in 2013 discovered the first shared codes in microRNA secreted by a type of human white blood cell. García’s team has identified more codes that tell cells to secrete microRNA and, for the first time, uncovered the existence of code that tells the cell to retain it. “These sequences instructing [the message] to remain in the cell can also be of great clinical use,” said the researcher.
Some types of medication are already using molecules similar to microRNA to treat certain diseases. Inclisiran, made by the Swiss pharmaceutical company Novartis, reduces the amount of cholesterol in the blood by inhibiting cell production of a protein that raises these levels. García believes it is possible to modify this type of molecule by adding barcodes to make it remain longer inside the desired cells. “They could enhance the effects over time, so that medication would need to be injected less frequently,” he posited.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































