Theranostics: a new hope in the fight against cancer
The medical treatment, which combines therapy and diagnostics, has given terminal prostate cancer patients a 35% increased survival time in trials
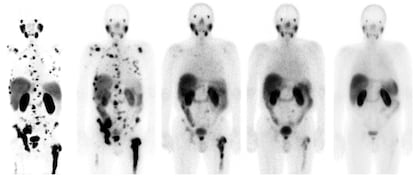
José Luis Carreras gets very excited when he talks about theranostics, a burgeoning medical strategy that works like a precision missile against certain types of cancer cells. Carreras, the head of nuclear medicine at the Hospital Clínico San Carlos in Madrid, speaks of “spectacular results” in some terminal patients, recalling the case of a 62-year-old German man with prostate cancer and a massive dissemination with metastasis in his bones. Eight months after an experimental treatment with theranostics at the Central Clinic Bad Berka in Germany, the patient’s cancer appeared to have gone. He returned to work and was playing sports again. Three and a half years on, he remains free of cancer, Carreras said in February at a conference at the Royal National Academy of Medicine in Madrid.
Theranostics was one of the main topics at the largest cancer conference in the world, held annually at the American Society of Clinical Oncology (ASCO) and this year conducted over the internet. The term theranostics comes from a combination of the words therapy and diagnostics: the same molecule can be used to both diagnose and treat the disease. The method, used for decades against thyroid cancer, is now being applied with promising results to other illnesses such as neuroendocrine tumors and, above all, prostate cancer, the most common cancer in men.
This is not the future; it is the present. It is personalized and precision molecular radiotherapyJosé Luis Carreras, Hospital Clínico San Carlos, Madrid
Michael Morris of the Memorial Sloan Kettering Cancer Center in New York presented the latest results concerning theranostics in the treatment of advanced prostate cancer at the ASCO conference. The technique consists of using a molecule designed to bind with high affinity to PSMA (prostate-specific membrane antigen), a protein that is generally present in large quantities in prostate cancer cells. To carry out the diagnostic, this PSMA molecule is combined with a radioactive chemical agent, Gallium-68, which glows in a PET-scan. For treatment, the same molecule is combined with another chemical element, lutetium-177, which emits localized radiation that kills cancerous cells. It is akin to firing an arrow with a lightbulb attached and then following that by an arrow with a small explosive charge.
Morris carried out a trial involving 831 patients with metastatic castration-resistant prostate cancer (MCRPC), a type of tumor that is commonly lethal. The patients that received theranostic treatment lived for 15.3 months, compared to 11.3 months among those patients who were administered standard treatment – a 35% difference. This may not seem like a lot, but the patients in the trial were terminally ill and had not responded to chemotherapy or hormonal treatments.
Carreras emphasizes that the extra four months of survival is an average. “There are cases where the patient doesn’t respond, but there are others in which the improvement is spectacular,” the physician says. His team at the Hospital Clínico San Carlos are due to participate in two clinical trials using theranostics against prostate cancer in September. “This is not the future; it is the present. It is personalized and precision molecular radiotherapy. You are not using a sledgehammer to crack nuts, as with other techniques. This is going directly to the tumorous cell, applying radiation and destroying it in situ without affecting the surrounding healthy tissue,” he explains enthusiastically.
Carreras believes that over the next few years molecules will be discovered “for every type of cancer,” such as Fibroblast-activating protein inhibitor (FAPI), related to the cells of various malignant neoplasms, or abnormal tissue growths. “Almost all tumors contain fibroblasts [a type of cell found in abundance in fibrous tissue] mixed with tumorous cells. With FAPI you can deliver radiation to the fibroblasts but, as the radiation range of lutetium-177 is one or two millimeters, it also destroys the tumorous cells. The advantage of FAPI is that it can be applied to any type of tumor,” says Carreras. But the physician notes that there is little evidence of the therapeutic efficacy of this technique, in part because of the low radiation dose delivered to the tumorous cells.
The success of this treatment highlights the importance of investigating alternatives to traditional cancer therapiesASCO President Lori J. Pierce
The promising experimental treatment presented to the ASCO conference, baptized 177Lu-PSMA-617, was being developed at US biopharmaceutical company Endocyte. Swiss pharma giant Novartis announced the purchase of Endocyte for €1.7 billion in October 2018. Some previous investigations, such as a 2016 study conducted among 30 patients at the Heidelberg University Hospital in Germany has already shown the potential of this treatment.
The oncologist Teresa Alonso of the Ramón y Cajal Hospital in Madrid believes that the benefit margin of this therapy “will certainly be much higher” if it is administered to patients in the early stages of illness. “The concept is not new, but now it is going to become quite fashionable,” says Alonso, who is also the scientific secretary for the Spanish Society of Medical Oncology. The researcher notes that it is a strategy similar to one used for decades against thyroid cancer, in which iodine-123 is used for the diagnostic and iodine-131 for the treatment. In recent years the same technique has been applied to neuroendocrine tumors, which have an annual incidence of fewer than 10 cases per 100,000 people. “Theranostics is a very nice concept and is extremely useful for the treatment of prostate cancer,” says Alonso, who nonetheless adds that people should not get too carried away: “This is not a cure for prostate cancer, obviously.”
The president of ASCO, US oncologist Lori J. Pierce, has greeted the results of theranostics against advanced prostate cancer enthusiastically. “The success of this treatment highlights the importance of investigating alternatives to traditional cancer therapies,” she said in a presentation. Morris, head of the medical oncology department at the Memorial Sloan Kettering Cancer Center, has suggested that US health authorities should study the possibility of approving 177Lu-PSMA-617 as a new standard treatment for prostate cancer patients.
Carreras, meanwhile, laments the “slowness” of the drug regulatory agencies when it comes to approving new therapies. One of the main problems is the high costs involved. Carreras estimates that theranostic treatment for a neuroendocrine tumor would cost €65,000 per patient. “It achieves a longer survival time than other alternatives and the price is competitive. It is no more expensive than the chemotherapy it would replace,” he notes.
English version by Rob Train.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































