Most lethal bacterium of all time became less virulent in order to keep killing millions
The evolution of a single gene from the bubonic plague microbe allowed it to survive for centuries — and to this very day
A bacteria measuring just one thousandth of a millimeter has brought humankind to its knees on three occasions. The first time, it was borne by rats in the heart of the Roman Empire during the year 541, killing thousands of people a day and leaving in its wake mountains of corpses in the streets. That was the Justinianic Plague, which was responsible for nearly 50 million deaths. The microbe violently reappeared in 1346, claiming the lives of one-third of Europe. The name of that second wave still sends chills down the spine: the Black Death. And the bacteria returned once again in 1855, spreading from the Chinese province of Yunnan to kill some 12 million people in the so-called third plague pandemic. An international team of scientists, led by Spanish microbiologist Guillem Mas Fiol, has discovered that the germ employed an unexpected trick to survive the centuries: it lowered its virulence to, paradoxically, be capable of more killing.
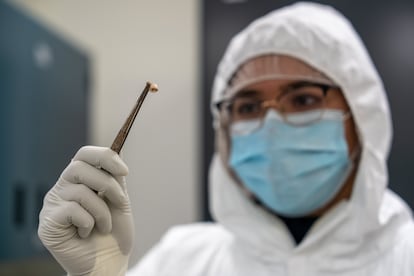
Mas Fiol, a 29-year-old born in the town of Felanitx on the island of Mallorca, Spain, works at the legendary Institut Pasteur in Paris, a few feet from the tomb of Louis Pasteur, the father of microbiology who upon his death in 1895 was buried at his own research center. In this very lab, the Spanish scientist researches live bacteria of the species Yersinia pestis, the culprit for the three plagues, which are among the seven most deadly that have struck the human race, along with the 1918 influenza pandemic, the arrival of smallpox to America, AIDS and COVID-19.
“There is a general theory that it could be more advantageous for a pathogen not to kill so many hosts, so that it can spread more, but that didn’t make sense in the case of the plague, because the plague needs to kill its hosts. It needs the pathogen to be in the blood, causing septicemia, so that when a flea bites, it finds the bacteria and can transmit it to another host,” explains Mas Fiol by telephone from Paris.

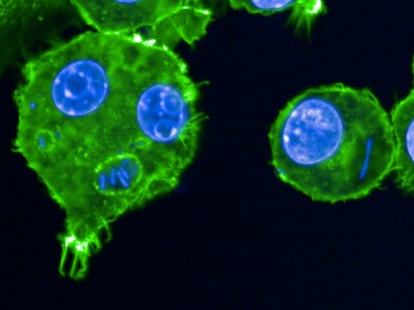
But upon analyzing microbial DNA recovered from hundreds of corpses of the victims of the three plagues, the Spanish researcher and his colleagues came across a surprising finding. The number of copies of a gene responsible for its virulence — which has been named pla — diminished with the passage of the centuries rather than increasing. The gene contains 938 base pairs and all the instructions necessary to manufacture a protein that allows the bacteria to travel to the lymph nodes and multiply before invading the bloodstream. The fewer copies of the pla gene the microbe has, the less deadly it is. Only, this is a pathogen whose survival depends on its lethality. “It was a puzzle,” recalls Mas Fiol, who works under the Costa Rican biologist Javier Pizarro Cerdá.
And so, the group experimented on rats: 20% fewer rodents died who had been infected with bacteria that had fewer copies of the gene. Those that did perish took longer to do so, with more time passing between infection and death. The researchers’ hypothesis is that natural selection favored less lethal strains, given that rats, its usual reservoir, are scarce after waves of mass rodent mortality. By simply modifying the number of copies of the gene, evolution had caused the bacterium to lower its virulence so that it didn’t kill all of its hosts. Thus, it persisted over time, spreading among fragmented populations, and wound up killing even more people. The results of the team’s investigation were published Thursday in Science, a leading international scientific publication.
The third plague pandemic, which began in China in 1855, according to the study’s authors, “continues today” in endemic regions such as Uganda, the Democratic Republic of Congo, Mongolia and the United States. The U.S. National Institutes of Health report that, before the existence of antibiotics, 60% of people infected with the plague in the country died. Now that mortality rate is 11%, thanks to drugs like ciproflaxin and doxycycline. “Almost all people with septicemic and pneumonic plague die if not treated immediately,” warns the institution. Septicemic plague, a generalized blood infection that occurs when bubonic plague is not treated in time, causes bleeding from the skin and organs, diarrhea, vomiting, extreme weakness, and tissue death. The skin turns black and dies, hence it being known as the Black Death.
“Reducing its virulence allowed it to persist longer in host populations that would not have supported a 100% virulent Yersinia pestis. It is a way for transmission in the pandemic to last longer. We had never seen this characteristic in plague before. It evolved to be able to persist for longer. It was an adaptation made out of desperation,” summarizes Mas Fiol, lead author of the study alongside geneticist Ravneet Sidhu of McMaster University in Ontario, Canada.
Microbiologist Bruno González Zorn, a professor at the Department of Veterinary Medicine at the Complutense University of Madrid, applauds the new study, in which he did not participate. “This leaves us with a crucial lesson: the number of copies of a gene can modulate the virulence of a pathogen. It is not just the presence or absence of a virulence factor that matters, but how many times it is present and where. This concept is key to understanding not only the plague, but also the evolution of antibiotic-resistant bacteria today,” says González Zorn, who is an advisor to the World Health Organization on antimicrobial resistance.
The professor explains that many resistance genes are spread in plasmids, small circular DNA molecules found in bacteria. González Zorn’s laboratory has shown that the accumulation of these plasmids, each with a resistance gene, can lead to the phenomenon of multi-drug resistance: superbugs that survive all antibiotics.
“Ecological context is also important: when the plague killed millions of rats, the selective pressure changed. A very virulent strain was no longer efficient: a milder strain was preferable, one that gave the vector or host time to reach new foci. This is a perfect example of the One Health approach: the interaction between ecology, bacterial genetics, animal and human health, all at the same time,” says González Zorn. “In a world where resistant bacteria travel on planes, in wastewater and in meat products, understanding that a simple variation in the number of copies of a gene can alter its pathogenic behavior is essential. It can mean the difference between a controllable infection and a new pandemic,” he says.
Sign up forour weekly newsletterto get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































