The man who was bitten hundreds of times by poisonous snakes paves the way for a universal antidote
A scientific team has created a serum that neutralizes the venom of 19 of the most lethal species, such as the black mamba or the king cobra, using the antibodies of an American man who nearly died due to his obsession with these animals

Every year, between 81,000 and 138,000 people worldwide die from complications resulting from snakebite venom. These deaths are silent, often occurring far from hospitals, in rural areas of the Americas, Asia and Africa. The most disturbing thing is that the antidote currently used is not so different from the one created by French physician Albert Calmette in 1895: a serum derived from immunized animals.
More than a century later, a group of U.S. scientists has taken a promising step by developing and testing an antidote in mice, with encouraging results. The antivenom has the potential to protect against the bite of lethal species such as the black mamba, the king cobra and the rattlesnake, according to a new study published this past Friday in the journal Cell. But the most surprising aspect of the discovery is its origin. The new formula was developed partly by using the antibodies of Tim Friede, a former truck mechanic from Wisconsin who has spent 18 of his 56 years voluntarily immunizing himself against snake venom. And he has done so by receiving bite after bite. More than 200 bites in total, plus 700 progressively larger doses of venom that he self-administered.
Friede’s story is both absurd and admirable. He’s no scientist, but his body has become a living laboratory. And from his own antibodies — shields he has literally been building himself with his immune system — now springs hope for a new generation of antidotes. The experimental serum combines two of those antibodies with a small-molecule inhibitor, which could pave the way for a universal antidote. The discovery was led by Jacob Glanville, CEO of the California-based vaccine research company Centivax.
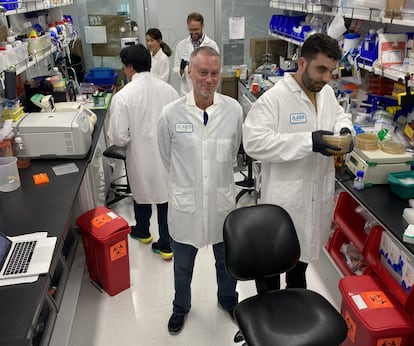
“I contacted Tim Friede and asked if we could get some of his blood to start looking into his immunological memory,” says Glanville, senior author of the study. Key to their success was the expertise of Peter Kwong, a professor of medical sciences at Columbia University and a member of the National Institutes of Health. The two scientists met at the Gates Foundation because they had received grants for the grand challenge of creating a universal flu vaccine. “The initial data Jake [Glanville] had on the inhibitor weren’t very encouraging,” admits Kwong.
Glanville had discovered the antibody LNX-D09 in Friede’s blood, which initially protected the mice from a dose of venom from six of the 19 most lethal species of elapids — whose neurotoxic venoms primarily affect the nervous system, causing paralysis and other complications. “But when they added the third component, they got much better, and that’s what’s described in the current paper,” Kwong says. The team added the small molecule varespladib, a known toxin inhibitor. They also included a second antibody isolated from the donor, called SNX-B03, which extended the unprecedented full protection against 13 of the species and partial protection against the remaining ones.
Although there are more than 650 types of snakes in the world, their venoms are based on a limited number of toxins. “We have managed to identify a method for adding compounds that can neutralize different types of toxins at the same time. This allows us to design an effective therapeutic cocktail,” says Glanville.
Tom Friede’s obsession brought him to the brink of death on several occasions. That’s why scientists emphasize that no one should replicate this behavior. The ethical framework for the study was based on HIV research, where high-risk individuals are sometimes studied, but they are not exposed to a higher risk. “We never gave him an antidote; we just drew his blood,” Glanville notes.
Towards a universal antidote
When a person receives a dose of traditional serum, they can suffer many dangerous side effects, and its effectiveness can vary by region. Jacob Glanville grew up in Guatemala, in a Mayan village called Zutwil. In communities like that, farmers spend their days working the crops, others go out to cut firewood, and many homes are located very close to the forest or jungle. In that context, it’s not uncommon for snakes to wander into backyards.

A child receiving traditional treatment, Glanville notes, could avoid anaphylaxis but still develop serum sickness, a severe immune reaction. This is where the new antibody cocktail stands out. “It is designed to be administered intramuscularly, which would facilitate its use in rural settings. Furthermore, it doesn’t require precise identification of the snake species and could be administered immediately,” he points out.
María Elena Barragán, executive director of the Gustavo Orcés Herpetological Foundation in Ecuador, believes the study is necessary and valid, as it “shows a path forward,” although it would still take some time before something similar could be adapted to Latin American countries. “The incorporation of molecular analyses, which are replicated in laboratories specializing in nanotechnology and nanomolecules, is being led by developed countries such as the United States, Australia, and England,” she maintains.
“The goal is precisely to advance in areas where countries like ours are required to have species management and conservation centers,” she argues. Eighteen species of vipers from the genus Bothrops (commonly known as X-snakes) and another 18 from the genus Micrurus (corals) have been identified in Ecuadorian territory, which are related to the group of elapids analyzed in the study. According to the herpetologist, at least 10 years of research and trials would be needed to effectively disseminate this information to society and authorities. “Clearly, this could be the starting point,” she concludes.
Experts acknowledge that the experiment has limitations. The mice were given a dose of venom four times the lethal dose, which guarantees death if the antivenom doesn’t work. In a real bite, however, the dose varies and can even exceed that amount. “We plan to repeat some experiments with more venom to detect other relevant toxins,” the expert says. They also hope to develop an antivenom targeted at the other major family of snakes: vipers.
Next step: trials on dogs
After testing their antivenom cocktail in laboratory mice, the team now seeks to test its effectiveness in the field, starting by administering the antivenom to dogs brought to veterinary clinics for snakebites in Australia, where venomous snakes are abundant. There, humans and dogs are bitten by the same species. Dogs are ideal candidates for controlled trials in veterinary clinics.
The advantage of these snakes is that their venom causes progressive paralysis without damaging tissue, allowing the antidote’s effect to be clearly observed. “If it doesn’t work, you can resort to standard treatment without putting your pet at risk,” says Jacob Glanville. This strategy would allow the new antidote’s effectiveness to be demonstrated in a real-life setting before moving on to human trials.
The next steps don’t depend on academia, but on industry, says Peter Kwong. “You need a company that brings all of this together and creates a product that can be sold to people,” he says. It all depends on the funding they can secure.
Scientists hope this breakthrough can soon be applied to humans and its effectiveness extended to other types of snakes, thereby reducing deaths from envenomation. “What we present in the publication is a roadmap, a method for combining — one by one — a series of broad antibodies or other components to neutralize toxins. We have begun that process,” Glanville reflects.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































