CAR-T cancer treatments: From science fiction to saving lives
The innovative therapies are currently being used in a very small number of patients but early results have been spectacular, offering real hope for people who have exhausted all other possibilities
Joan Gel, a 67-year-old resident of Mataró, Barcelona, last December told EL PAÍS how his life had been saved by innovative cancer treatments. Gel had been suffering from multiple myeloma, a type of blood tumor, for 12 years and had been treated with experimental therapies at the Hospital Clínic in Barcelona along with 30 other patients who had run out of conventional options. Blood was taken from all the patients to obtain their T-lymphocytes – a type of cell that defends the body from various threats, among them infections and tumors – to modify them with genetic engineering. The aim was to improve their own white blood cells so that they would be capable of recognizing the cancerous cells that caused the myeloma. Of the patients, 18 of them (60% of the total) experienced complete, if not necessarily indefinite, remission of the disease.
Great medical innovations tend not to be confused with science fiction when they eventually reach patients, but this kind of treatment, known as CAR-T (T cells with chimeric receptors for antigens) certainly seemed to be for decades. Carl June, a University of Pennsylvania scientist and one of the pioneers of this type of therapy, began to believe it could be made a reality after his wife was diagnosed with ovarian cancer in 1996. Earlier this month, June and several co-authors published an article in Nature with the results of a decade-long follow-up of two of his first patients, Bill Ludwig and Doug Olson, who were first treated in 2010. Despite his reticence to use the word when discussing cancer, June considered them cured.
Over the past two decades, the work of several investigative teams, first in the US and then in other countries, has turned what were previously experimental therapies into a genuine chance for ever-more patients. The treatment that saved the lives of Ludwig and Olson in 2017 became the first CAR-T approved for commercial use in the United States. Developed by pharmaceutical giant Novartis, today it is known as Kymriah.
At the moment, like many cancer treatments in their early stages, it is proving useful mainly against blood tumors like leukemias and lymphomas, and principally in patients for whom all other therapies had been exhausted. This happened previously with chemotherapy and targeted treatments that are now in large-scale use as the primary option against all kinds of tumors. Since 2019 in Spain, fewer than 500 CAR-T treatments have been approved, a drop in the ocean compared to the 270,000 tumors diagnosed each year. However, the success of this treatment in its first few years has led to calls to widen its use.
Joaquín Martínez, head of the Hematological Malignancies Research Unit at 12 de Octubre Hospital in Madrid, who has participated in international studies to broaden the indications for these products, explains that one of the steps toward expanding the use of CAR-T is “bringing forward the moment in which it is applied, because the lymphocytes are healthier and the results will be better.”
Furthermore, it is hoped that CAR-Ts will also work against solid tumors, such as those in the colon or mammary, which are far more common but also much more complicated to treat from a genetic or biological point of view. “In total, between 40% and 60% of hematological tumors, perhaps not in the early stages, but at some point, could receive this kind of therapy,” says Felipe Prósper, head of the Advanced Therapies Unit and co-director of the Hematology and Hemotherapy Unit at the University of Navarre. “They will have a high uptake in these minority diseases, but if we were able to transfer it to solid tumors, the numbers would be much higher and difficult to manage.”
What Prósper is referring to is a common problem among many of the most successful advanced therapies in modern medicine, among which CAR-T is at the vanguard.
Reducing the time between when the treatment is approved to the time when the cells are reintroduced is very important, because with CAR-T, time has a very significant impact on the subsequent responseJoaquín Martínez, head of the Hematological Malignancies Research Unit at 12 de Octubre Hospital
The treatments Kymriah, as well as Yescarta from the biopharmaceutical company Gilead, have been approved in Spain and cost around €300,000 ($340,000) per patient. But even those CAR-Ts developed in hospitals, such as the one at Barcelona’s Hospital Clínic, can cost over €100,000 ($113,000) per treatment, among many other reasons because their creation requires an almost artisanal touch and highly, and very specifically, trained personnel. The scientific and technological challenges that lie ahead, as well as the political and financial, are considerable.
According to data from the latest report on the plan for the approach to advanced therapies by the Spanish Health Ministry, dated June 2021, of the 497 requests for CAR-T treatment that have been made since its arrival in the country in 2019, 435 have been approved: almost 90%. However, only 244 of the patients who were given approval actually received the treatment. In a patient group who tend to be already very ill, the time it takes to carry out the process – as much in terms of administration as in technical concerns – can mean the difference between life and death. This is another area experts say can be improved. “Today in Spain, from when the treatment is approved to the time when the cells are reintroduced takes around 60 days. Reducing this time scale is very important, because with CAR-T, time has a very significant impact on the subsequent response,” says Martínez.
To try and ensure that innovative drugs do not represent a crippling cost for the public health system, the Spanish government has negotiated a system of shared risk with the pharmaceutical companies, through which the total price of the product will only be paid if pre-determined results are obtained. Furthermore, some experts note that other cancer treatments can cost over $100,000 per patient. The financial aspect represents a clear challenge to expand the availability of these therapies, but physicians believe it is essential to recognize their inherent value.
Regina Quiroga, Gilead’s medical director of cellular therapy, points to success stories like the one recently presented by her company at the American Society of Hematology congress. “In diffuse large B-cell lymphoma, in patients that previously had a life expectancy of six months, we are now seeing that almost 50% [42.6%] are alive,” says Quiroga. Now, she adds, is the time to bring treatments such as these in line with previous treatments so they can be applied in more hospitals.
Quiroga does not go so far as to suggest bringing forward technological developments under development at companies to bring down costs and make these therapies more accessible, but there are groups the world over who are working in that direction. Prósper says that he and his team are looking for alternatives to the genetic engineering required to modify T-lymphocytes. As it stands, viruses are used as a means to transport the necessary modifications into cells for them to attack tumors. The team at the University of Navarre wants to substitute this method for transposons, so-called “jumping genes,” which are DNA sequences that are naturally capable of changing their place in the genome, and which could serve to introduce sequences in the lymphocytes to enable them to attack tumorous cells. According to Prósper, this technology, if it proves to be effective, could improve the safety profile of the process and make it cheaper.
Improving the safety profile at the same time as increasing potency are key elements in future work on this kind of cell therapy and other similar treatments in the advance toward being able to apply them to solid tumors. “There are few bullseyes for CAR-Ts that allow for the creation of a cell therapy that attacks the tumor without damaging healthy tissue. Toxicities are a limitation,” says Alena Gros, head of the Immunotherapy and Immunology Department at the Vall d’Hebron Institute of Oncology in Barcelona.
Between 40% and 60% of hematological tumors, perhaps not in the early stages, but at some point, could receive this kind of therapyFelipe Prósper, co-director of the Hematology and Hemotherapy Unit at the University of Navarre
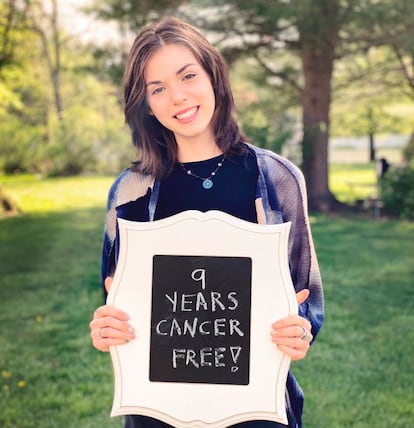
In 2011, Emily Whitehead, a six-year-old suffering from leukemia, had a relapse after 16 months of chemotherapy. She was one of the first people to receive CAR-T treatment. At the time, her immune system’s response was on the verge of killing her, but tocilizumab, a monoclonal antibody that is used for arthritis, was able to keep it under control. Had Emily’s case gone badly, as happened with some of the first attempts to apply genetic therapies to such cases, it could have set CAR-T treatments back by at least 10 years.
This control of toxicities will be a key element in the success of making the jump to solid tumors. At the Vall d’Hebron Institute, Gros and her team are working with TIL (tumor-infiltrating lymphocytes), a technique with similarities to CAR-T. “We remove the T-lymphocytes that have infiltrated the tumor and screen them to see which ones better recognize the tumor or any mutations,” she says. These cells, which are especially useful in the fight against cancer, are multiplied and re-introduced into the patient. “It is a treatment that is still experimental, but it has yielded interesting results in melanoma and in some cases of breast cancer,” adds Gros. This technique, developed by surgeons at the US National Cancer Institute, another CAR-T pioneer, has delivered some spectacular results, like the case of Judy Perkins. In 2014, Perkins was diagnosed with metastasized breast cancer and physicians gave her two months to live. Today, she is still alive.
Gros and other physicians at the vanguard of this revolution in cancer treatment say it is important that patients “know that these options exist,” although they also sound a note of caution over spectacular results like those of Perkins, Ludwig and Olson, stressing that these therapies are in their infancy. However, the history of the fight against cancer provides reasons for hope. In the 1960s, a large section of the medical community considered chemotherapy treatment an aberration. In the 1970s, with the first treatments available, over 50% of children diagnosed with blood tumors survived and today the rate of survival five years after being diagnosed stands at over 80%. Many of those children, who were involved in the first oncological revolution, are today the greatest testament to its success.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































