How a leukemia patient was cured of HIV thanks to umbilical cord blood
The case has been described as rare and the treatment unlikely to be applicable to most people living with the virus, as it is only ethical to perform this transplant on people with hematological cancers
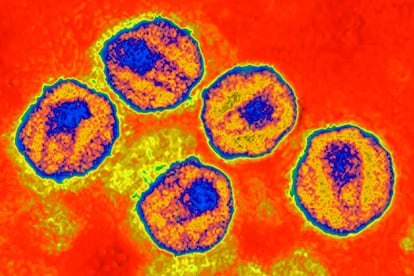
An American research team has announced that for the first time, a woman with HIV appears to be cured thanks to an umbilical cord blood transplant. The patient received the treatment in an attempt to treat her leukemia. The procedure against this blood cancer seems to have eliminated the virus from her body, as announced by her doctors at a conference on retroviruses held in Denver, Colorado whose conclusions have been reported by The New York Times.
This case is now the third where patients were declared to be “in remission,” as researchers are normally reluctant to say “cured.” The first case was Timothy Brown, known as “The Berlin patient,” who stayed HIV-free for 12 years after a stem cell transplant (he died of cancer in 2019). The second case, also involving a man, was announced in 2019. An international consortium that included the IrsiCaixa AIDS Research Institute in Barcelona identified a patient whose doctors stopped his anti-retroviral treatment after a stem cell transplant. The virus has been undetectable in his blood for three and a half years.
In the woman’s case, doctors withdrew conventional antiviral treatment 37 months after the transplant. One year and two months later, there is no trace of HIV in her blood and no antibodies against the virus.
The most striking thing about this remission is that the patient, whose age and name have not been disclosed, received a different type of transplant than the two previous cases. Both men underwent bone marrow transplant from adult donors that fully matched their own immunological profiles. In both cases, the donors had a mutation in the CCR5 gene that confers resistance to HIV infection. Blood stem cells from the donors’ bone marrow ended up replacing the patients’, shrinking their hematologic tumor and giving them resistance to HIV. The third patient, on the other hand, received cord blood from a donor who also had the beneficial mutation. The mechanics of stem cell replacement was the same, but in this case the compatibility with the donor was lower.
It can take months for this type of procedure to take effect, so doctors also resorted to a transfusion of blood stem cells taken from a close relative of the patient to improve the chances of success. This probably strengthened the patient’s immune system until the cord blood transplant took effect, which in turn reduced the risk of the operation, according to Marshall Glesby, a doctor at Cornell University in New York and a member of the American research team. The two previous cases suffered major complications after the transplant, but this woman was able to leave the hospital 17 days after surgery.
We have to remember that the mortality rate associated with this type of transplant is 30%, so it should only be applied to people with hematological cancersJosé Alcamí, Carlos III Health Institute of Spain
This milestone is also important because the patient is a woman. Some studies have detected a different progression of the HIV infection in men than in women, but despite this, women are a minority in clinical trials of new treatments against this infection.
José Alcamí, head of the AIDS Immunopathology Unit at the National Microbiology Center of the Carlos III Health Institute in Spain, explains the importance of this new case. “In this case, umbilical cord cells that were removed after birth and stored frozen in biobanks have been used,” he says. “In bone marrow transplants, the donors are adults and therefore there must be full compatibility between donor and recipient. If we add to that the need to have the mutation in the CCR5 gene, we find that compatibility only happens in one case out of six million. In contrast, with cord blood, compatibility can be less than 50%, which increases the chances of finding a suitable donor.”
In any case, it will be difficult to extend the scope of this treatment to the many people living with HIV, since it is only ethical to perform this type of transplant on people suffering from hematological cancers such as leukemia, Alcamí warns. “We have to remember that the mortality rate associated with this type of transplant is 30%, so it should only be applied to people with hematological cancers. Another thing to consider is that cord samples with the mutation in the CCR5 gene should be reserved in case they can be used in the future for another patient who also has HIV. This is a very spectacular case, but unusual”, he highlights.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































