Inside the Spanish lab seeking the definitive Covid-19 vaccine
Luis Enjuanes should be retired by now, but he is heading a team of 16 people trying to develop complete immunization from the coronavirus
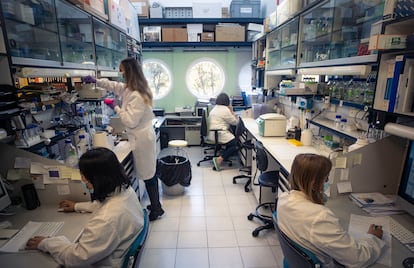
One of the world’s leading experts on coronavirus, Luis Enjuanes, works out of an office no more than five square meters in size. On the second floor of the National Biotechnology Center (CNB) of the Spanish National Research Council (CSIC), in Tres Cantos, Madrid, he has a team of 16 people working in the laboratory outside his door, where the search for a vaccine that provides sterilizing immunity against the coronavirus began almost two years ago.
If there is one thing scientists don’t like, it’s answering the question most loved by journalists: “When could it (in this case, the vaccine) be ready?” There are so many factors that influence how research pans out that predicting its success often leads to mistakes. Initially, Enjuanes’ team thought they might have the vaccine by now. But there have been obstacles. At this point, “if everything goes to plan,” Enjuanes is speaking about one more year. “Luckily, vaccines are no longer as urgent as they were at the beginning of the pandemic,” he says.
For Enjuanes’ team’s vaccine to be worthwhile, it must contribute a characteristic lacking in those that already exist. This could be sterilizing immunity, meaning those who get the vaccine neither become infected nor infect others. The most effective way this can be administered is via a nasal application. “If you use intramuscular injection, either in the arm, in the thigh or in the buttock, it provides a systemic, internal immunity, which lasts for 20, 40, 60 years and a single dose is good. However, it is not what we need right now; what we need now is immunity that protects the mucous membranes,” he says.
The problem with intranasal vaccines is that getting them approved is complicated. Regulatory bodies subject them to strong safety measures, as they fear that some component of the drug might cross the blood-brain barrier – the one that protects the brain from harmful substances – and cause unwanted side effects.
Enjuanes maintains that this possibility is minimal and that there are other drugs that are applied through the nose without this happening. But since it is not “the health authorities’ preferred method,” they are working on two versions of the vaccine; one, intranasal and the other, intramuscular. “I am convinced that if they could administer the same Pfizer or Moderna vaccine intranasally, two doses would not be necessary,” he says. “And the people who got it would not get the virus. And if they did, it would not replicate and they would not pass it on to other people.”
In the race to launch the first effective vaccines, Pfizer-BioNTech, Moderna and several other brands, such as AstraZeneca, were first over the finishing line. Janssen, which arrived a little later, had to provide something the others lacked, which turned out to be that it did not need to be stored at extremely low temperatures and it required (in principle) a single dose. Vaccines against Covid-19 will continue to evolve and adapt, bringing improvements, but there will no longer be the urgency that was there initially when it was imperative that something be found to put the brakes on an explosive pandemic ripping through an un-immunized global population.
There are more than 300 coronavirus vaccines currently being researched. Of these, 135 have reached the stage of being clinically tested on humans. Among the half-dozen that are being developed in Spain, the only one that has reached this stage has been developed by the pharmaceutical company Hipra. It is in phase II-B and is being tested on 1,000 volunteers to verify its safety and efficacy as a booster.
Enjuanes and his team aim to test their vaccine on people early next year. “The first and second [clinical phases] are economically very feasible even for our economy, our laboratory and our institution – the CSIC – because you can cover that with €4 million or €5 million,” says Enjuanes. “But phase 3, which involves up to 60,000 people, costs millions. And you can only do that in collaboration with a major company. We are in talks with a company that has a lot of scientific experience and great potential,” adds Enjuanes, who would be retired if it were not for the pandemic.
Three levels of security
The team uses CNB facilities, allowing them to work in laboratories with three levels of security. Level 1 is distinguished by its yellow door. With little space between researchers, they build mutants of the coronavirus in which they isolate genes that mitigate its virulence in order to develop future vaccines. On a dish, Enjuanes shows how the cells infected by the virus disappear and those that do not become infected remain visible, a sign that there is an immune response.
Level 2 has orange doors. Here, researchers work with microorganisms that would not be able to infect humans even if they escaped. However, to enter, you have to go through an airlocked compartment and put on a gown that is kept in the room at all times.
The jewel in the crown at CNB is the 3+ security laboratory – the highest is Level 4 by international standards. The door is red, and resembles the door to a submarine. A camera monitors those entering and leaving the premises. Dangerous pathogens are handled inside and the measures to keep them there are extremely strict.
Here, the pressure is negative: when the door opens, air enters but does not leave. Anyone going in must wear airtight clothing and breathe through a filter: this is what differentiates the space from Level 4, where oxygen is supplied by a cylinder. Inside the laboratory, the air is filtered and each researcher is isolated within their own cubicle. Only those authorized to do so can access Level 3.
“This is where we assess the mice after they have been subjected to a lethal dose of the virus, for example,” Enjuanes explains. “And we see if the vaccinated mice survive compared to the unvaccinated ones.”
For the time being, they can only test on animals. If the safety data in macaques is good, they will try to make the leap to the clinical trial phase. But there is still a long way to go; more than 85% of the drugs that reach phase 1 fall by the wayside. The good news is that vaccines against infectious diseases have a better prognosis: a third of those that reach human trials end up being approved.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































