Artificial intelligence is put to the test with the health of populations in the Global South
From depression to malaria to meningitis, digital image processing and language algorithms can help detect and prevent widespread and neglected diseases. However, researchers agree that everything still depends on the human factor
To a large extent, it all depends on the quality of the image. With a clear photograph, it’s possible for a medical professional to know if an affliction is, for example, Buruli ulcer, leishmaniasis or leprosy.
There’s a mobile application that allows for the effective and early detection of neglected skin diseases. Integrated into the phone, it uses artificial intelligence (AI) to screen — among the enormous variety of ailments — those with the highest incidence in many developing countries, where they affect more than one billion people in total.
Dr. José Postigo is from Catalonia, in northeastern Spain. He works with skin diseases in the Department of Control of Neglected Tropical Diseases (NTDs) at the World Health Organization. He’s leading this AI project and hopes to demonstrate its effectiveness in Kenya during the first months of 2024.
“Our application is designed so that it can be used by both clinical staff and community agents at primary healthcare levels,” explains Postigo, from the Dominican Republic, where he is attending a dermatology conference. “So far, we’ve received images from organizations that work in several countries in Africa and Latin America. [The] AI compares and analyzes images. It replaces the eye of the dermatologist.” And, if the staff taking the photos requires more guidance, the app displays a menu of 12 highly prevalent NTDs in developing countries.
According to Dr. Postigo, the NTD Department is a pioneer within the WHO when it comes to betting big on the use of AI. “We have to see the application’s effectiveness… if it’s approximately 90% correct, it will allow us to get results in a second. This surpasses telemedicine and teledermatology in terms of response times. [It will also be] much more sustainable.”
This is an example of the various apps that use AI, which are being developed to bolster the health of populations with limited resources. At the moment, early and accurate detection is the great contribution that AI can make to medicine. However, while we’re witnessing its development, researchers agree that, for now, everything still depends on the human factor, which is behind the data collection and the subsequent analysis of said data. “For our application to work, a large number of images is needed to achieve greater screening accuracy,” Postigo notes. “This requires the participation of health personnel and community agents from the countries where these diseases have the greatest impact on the population.”
AI sees what nobody else can
Meningitis is due to inflammation of the tissue that covers the brain and spinal cord. It can be of viral or bacterial origin. It’s a very serious and lethal disease for babies if it’s not treated in time. This is especially the case in sub-Saharan Africa, where the incidence is 1% and the mortality of children is between 5% and 20%. The usual diagnosis for meningitis in babies is based on a lumbar puncture.
Paula Petrone is an Argentine biophysicist. She is the head of the Biomedical Data Science working group at the Hospital Clínic de Barcelona. “As a mother,” Petrone says, “I wish doctors would use less invasive methods than a lumbar puncture.” According to her, the question is: “Are there less invasive and expensive ways to diagnose meningitis?” She tells EL PAÍS that AI has the answers.
Petrone’s team is collaborating with the Barcelona-based start-up Kriba.ai on the application of a portable device, which is a high-resolution, ultrasound-based white blood cell counter. With the assistance of AI – which analyzes ultrasound images – meningitis is detected quickly and easily, if the count is high. If the count is normal, this means that the absence of the disease is detected risk-free, without the need for such invasive methods.
To do this, the device scans the baby’s brain through the fontanelle (a soft spot on the skull). “The images it takes are of very high resolution and [are sensitive] to the presence of cells... but they don’t allow radiologists to see where the white blood cells are. However, the algorithm can distinguish meningitis in an image, while we cannot,” Petrone notes.
The device is easy to use and maintain and, therefore, it enables screening anywhere in the world. According to its developers, this is particularly important in countries where there’s a shortage of trained personnel and laboratories. At the moment, it’s being validated in Morocco and Mozambique.
For Petrone, the potential of AI lies in the early detection of diseases, whenever current diagnostic methods aren’t effective, or are too expensive or invasive. “In our research group, we’re betting on the application of deep learning techniques for the identification or classification of patterns in medical images. In this field, for example, the use of AI in detecting schistosomiasis (a disease caused by parasitic worms) is promising. The aim is to more accurately identify eggs in stool or urine samples, or – in diseases such as chagas or malaria – detect parasites in blood samples.”
The main source of funding for these projects comes from the Bill and Melinda Gates Foundation. And, for the meningitis project, the Spanish Agency for International Development Cooperation (AECID) has joined forces with private financing and the European Innovation Council Accelerator. Petrone’s work is funded by the Spanish Ministry of Science and Innovation, through the Severo Ochoa Center of Excellence.
One of the most important aspects that Petrone highlights is the participation of scientists and researchers from countries where many of these diseases are prevalent. Her team works with professionals from Mozambique, Ethiopia and Argentina, among other nations, to diagnose childhood tuberculosis or Chagas disease.
Addressing the double burden of disease
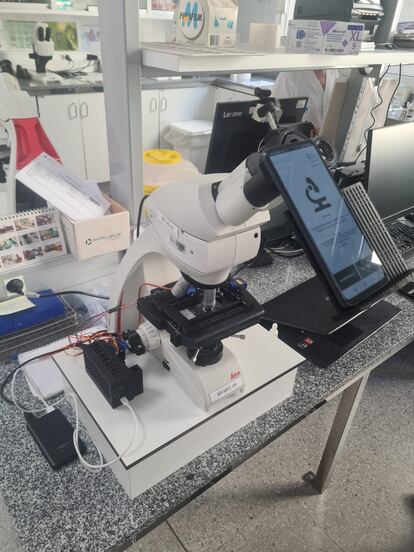
Malaria can be detected more quickly via imaging. There’s a mobile application that – using a low-cost microscope equipped with an Arduino computer – analyze samples quickly and efficiently. Daniel López Codina – a biophysicist at the Technical University of Catalonia (UPC) – is leading this project. He explains that automatic detection of malaria parasites can be achieved through AI techniques based on deep neural networks. All of this reduces the resources and time that the most affected countries have to dedicate to analysis. With the support of the Probitas foundation and the collaboration of the Vall d’Hebron Hospital and the UPC, this application could work not only for malaria, but for diagnoses of various pathologies that can be detected by microscope, according to López Codina.
In developing countries, chronic pathologies are advancing with the increase in life expectancy. This represents a challenge for health systems that have to face them, along with other highly prevalent infectious diseases. “It’s about the double burden of disease,” says Jordi Serrano, a family doctor and entrepreneur in digital global health. He’s the founder of the UniversalDoctor platform, which has developed technology to support the WHO in the face of the Zika virus, mental health crises and other issues.
Serrano also collaborates with Dr. Postigo’s department in the development of the application for skin diseases. He emphasizes that, in the affected countries, there’s a need for a greater number of images and improved collaboration with health personnel. “This is vital, so that AI can be used to screen many pathologies with similar symptoms.”
When the application developed by Serrano’s team for the WHO is tested in Kenya, it will be known whether or not “the AI truly works and is useful where it’s needed,” Postigo explains.
The human factor
AI is based on the creation of neural networks, something that, in other words, imitates the human brain. Mariano Sigma – an Argentine neuroscientist – explains how AI works, through its enormous computing capacity. It offers us alternatives that we didn’t previously have to predict and diagnose diseases.
Sigman explains this by referencing a tennis match. Two sports legends from the 1990s faced each other at Wimbledon: Andre Agassi and Boris Becker. “Becker was a great server and Agassi was a great returner. The player who serves tries to do so in such a way that the opponent cannot decipher where the ball is going to go… but Agassi noticed something Becker was doing with his tongue. He put it in the position where the ball would go. That, of course, gave him a huge advantage in responding to the serve. This is how a neural network works, more or less,” he summarizes, during his presentation at a symposium on global health in Buenos Aires.
The neuroscientist foresees great possibilities for the use of AI in global health. He has already observed the potential in the field of mental health. “An example of application is in the case of depression. Drugs – as in other pathologies (cancer, for example) – work well in some people and not in others, without us knowing why in many cases. AI can help predict which people will respond best to [each respective] treatment.”
For Sigman, the big leap has come recently, with AI being able to use human language. In the field of psychiatry, this allows for great progress, since the primary source of information is usually the oral interview with the patient.
The neuroscientist recalls that some studies have revealed a “surprising paradox” when comparing conversations between mental health patients with their human therapists and those maintained with AI. In some cases, patients perceived conversations with the AI as more effective and empathetic than those they had with the human therapist.
What does AI have to say about this?
Something missing from the conversation is what the AI itself has to say on the subject. Upon asking ChatGPT what AI could do to combat the most neglected diseases, its response was: “AI can play a significant role in the elimination of NTDs by contributing to various aspects of prevention, diagnosis, treatment and monitoring.” When asked for a specific example, ChatGPT pointed precisely to the diagnosis of skin diseases.
Researcher Paula Petrone is clear: “Artificial intelligence isn’t here to replace doctors. They will always be needed from the point of view of empathy and a clinical eye. But these algorithms can definitely help us see things more clearly.”
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.








































