How babies develop during the first two years of life: A month-by-month guide
The scientific evidence on how an infant develops, socializes and feeds offers multiple data to take into account about the psychomotor evolution of children
Pediatricians call it the “thousand golden days:” the time that elapses between a baby’s conception and second birthday. Everything that happens during this period is crucial for the child’s future. The habits of the rest of the family, and the behavior and customs taken on board in the home, influence a baby’s metabolism and have a bearing on their future. As such, experts say, these months are the key moment in a baby’s life to promote healthy behavior.
This article is a chronology of the development of a healthy child born at term, according to the main pediatric societies and associations. But the milestones should not be taken too literally: what is described month by month is a reference, not a textbook. It is not a cause for concern if a baby is not walking after a year and not talking after 18 months. As the experts state, every child has their own timescale.
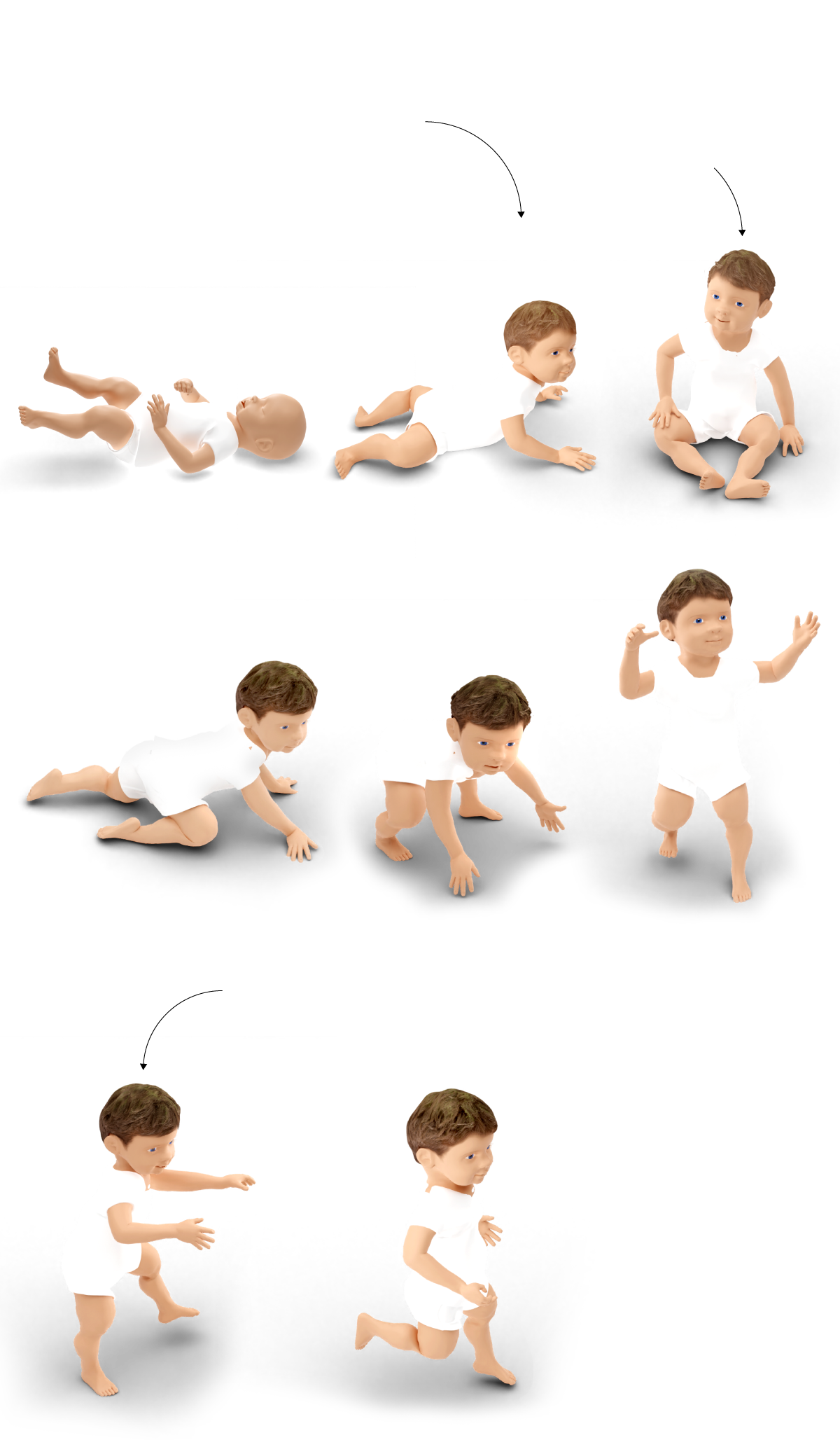
Physical changes: from lethargy to running
In these 1,000 days, a zygote measuring barely a millimeter turns into a child weighing 12 kilograms and who is running around everywhere, who talks more or less with ease, interacts with their surroundings, has feelings, laughs and worries. From birth, their brains become a sponge that absorbs everything around them. They learn to understand, to form relationships, to walk, to eat and to talk. And they do so at their own pace. The range of development “normality” is very wide and every baby is different, pediatricians stress. To begin with, a baby born prematurely and one born at term are not the same thing: the measurement parameters and rhythm of growth are different.

There are three motor milestones during
the first year of life
Month 0
Head control around
three months of age
Month 2
Lifts up
head
Sitting without support starts
at six to nine months old
Month 6
Able to sit
Month 8
Starts to crawl
Month 10
Stands up
Autonomous walking starts
at 12 to 19 months old
Month 12
First steps
Month 17
Starts to run
Starting the second year,
language development,
play and socializing play
a larger role
There are three motor milestones during the first year of life:
Sitting without support
starts at six to nine
months old
Head control around
three months of age
Month 2
Month 6
Able to sit
Lifts up head
Month 0
Month 10
Month 11
Month 8
Stands up
First
steps
Starts to crawl
Autonomous walking starts
at 12 to 19 months old
Month 17
Starts to
run
Starting the second year,
language development,
play and socializing play
a larger role

There are three motor milestones during the first year of life:
Sitting without support starts at six
to nine months old
Head control around
three months of age
Month 2
Month 6
Month 8
Starts to
crawl
Able to
sit
Lifts up
head
Month 0
Autonomous walking starts at
six to nine months old
Month 10
Month 11
Month 17
Starts to
run
Stands up
First
steps
Starting the second year, language development,
play and socializing play a larger role
In the first few months of life, the most mature structure is the brainstem, which governs the most basic functions: breathing and cardiac function. “Initially, a baby’s movements are reflexes, automatic, originating from the brainstem,” says Ana Camacho, president of the Spanish Society of Pediatric Neurology. “As other parts of the brain mature, such as the cerebral hemispheres, these reflex reactions start giving way to voluntary movements.”
This process is related to progressive cerebral myelination, says Camacho, a pediatric neurologist as Madrid’s Doce de Octubre hospital. “Myeline, which is essential for the proper transmission of nerve impulses, is present in small amounts at birth, and its increase, which is called myelination, occurs progressively from the lower to the upper areas of the brain, and from the posterior to the anterior zones. This process continues until the second decade of life, although at the age of two myelination is already well advanced.”
Everything passes through this enigmatic organ, which weighs just 350 grams at birth and doubles then triples its mass by the ages of one and two. Thousands of new neuronal connections are behind every step forward in psychomotor development and parents and pediatricians are obsessed with taking care of a healthy brain.
Care with the fontanelle
At birth, the bones in a baby’s cranium are not fused together: in the top and front zones of the head there is a diamond-shaped depression called the anterior fontanelle and at the back of the skull another triangular depression is visible. It is fine to touch these and perfectly normal that the skin covering the fontanelles rises and falls when the baby cries or strains.
As the bones that surround the fontanelles grow and join together, they make the depressions smaller until they close up. The anterior fontanelle tends to close between nine and 18 months and the one at the back of the head at around six months.

Posterior
fontanelle
Anterior
fontanelle
Baby
skull
Fontanelles are soft spots in the baby’s skull where the bones have not grown together yet.
They close between nine and 18 months after birth.
Before birth
Anterior
fontanelle
Posterior
fontanelle
During birth, the baby’s skull bones
move in order to get through the narrow
birth canal. The bones are still soft
and they go back to their normal shape
within a few weeks.
After birth
Anterior
fontanelle
Posterior
fontanelle

Posterior
fontanelle
Anterior
fontanelle
Baby
skull
Fontanelles are soft spots in the baby’s skull where the bones have not grown together yet.
They close between nine and 18 months after birth.
Before birth
After birth
Anterior
fontanelle
Anterior
fontanelle
Posterior
fontanelle
Posterior
fontanelle
During birth, the baby’s skull bones
move in order to get through the narrow
birth canal. The bones are still soft
and they go back to their normal shape
within a few weeks.

Posterior
fontanelle
Anterior
fontanelle
Baby skull
Fontanelles are soft spots in the baby’s skull where the bones have not grown together yet.
They close between nine and 18 months after birth.
During birth, the baby’s skull
bones move in order to get
through the narrow birth canal.
The bones are still soft and they
go back to their normal shape
within a few weeks.
Before birth
After birth
Anterior
fontanelle
Anterior
fontanelle
Posterior
fontanelle
Posterior
fontanelle
Face up or face down to sleep?
Parents today recall that when they were babies, their parents would always put them to sleep face down, without exception. Now, though, pediatricians recommend that babies sleep face up. Scientific opinion has changed and so too have the recommendations. Why? The risk of sudden infant death syndrome (SIDS) – which tends to affect children who are less than a year old – is key.

Recommended
FACE UP
Not Recommended
FACE DOWN
Risks
Asphyxia
Breathing in exhaled air containing CO2
Rise in body temperature

Recommended
Not Recommended
FACE UP
FACE DOWN
Risks
Asphyxia
Breathing in exhaled air containing CO2
Rise in body temperature

Recommended
Not Recommended
FACE UP
FACE DOWN
Risks
Asphyxia
Breathing in exhaled air containing CO2
Rise in body temperature
Premature birth, being around smokers, sleeping face down, being too wrapped up in blankets or sleeping in the same bed as parents all increase the risk of SIDS, says Cristóbal Coronel, president of the Spanish Society of Primary Care Outpatient Pediatrics (Sepeap). The causes of SIDS remain unknown, but the scientific community points to a combination of contributory genetic, environmental and sociocultural factors in what is a key period of neurological, cardiac and respiratory development.
Until the late 1980s, the recommendation was for babies to sleep face down, but in 1994 experts began to issue warnings about the risk of SIDS when sleeping in this position and urged parents to change to face up. Scientific papers suggest that sleeping face down increases the risk of SIDS by up to 14 times, mainly due to the risk of asphyxiation, but there are also other theories. For example, that sleeping face down can provoke oxygen deprivation leading to hypoxia, and the re-inhalation of carbon dioxide, which can lead to hypercapnia (abnormally elevated carbon dioxide levels in the blood). It can also compromise cerebral circulation, obstruct the airways, cause alterations in cardiovascular capacity or increases in body temperature, among other complications.
Walker or no walker?
A baby’s first unaided steps are one of the great developmental milestones in the first few years of life. And while there are toys designed to help them, like baby walkers, pediatricians are opposed to almost all such aids. Above all, the classic model that is like a small car with the baby sat in the middle, using their feet to propel it along. Laia Asso, head of the Catalonia regional government’s Intersectoral Public Health Programs for Children and Adolescents, says these toys can be extremely dangerous: “There are enormous risks on stairs if they fall. Because of the position the child is in, the upper body is exposed and the majority of the knocks are on the head.”

It’s not dangerous but it is
not recommended either
PUSH WALKER
Not recommended
WALKER WITH A SEAT
Risks
The child is not aware of their weight and inertia
It creates bad posture
The child does not develop reflexes

It’s not dangerous but it is
not recommended either
Not recommended
WALKER WITH A SEAT
PUSH WALKER
Risks
The child is not aware of their weight and inertia
It creates bad posture
The child does not develop reflexes

It’s not dangerous but is not
recommended either
Not recommended
PUSH WALKER
WALKER WITH A SEAT
Risks
The child is not aware of their weight and inertia
It creates bad posture
The child does not develop reflexes
Coronel of Sepeap adds that the height of the chair has to be precisely modulated due to the risk of curved feet. “The feet have to reach the floor correctly so that the legs are not suspended in parenthesis.”
Pediatricians are also not too keen on the hanging or bouncing walker, where a baby learns to take steps suspended from a kind of swing. Asso says they do little to help children learn to walk. “The baby starts to take steps without being conscious of their weight and inertia. You are not teaching them what it is to walk, with the wobbling and the insecurity.” Coronel agrees: “It builds bad posture and the child has all responsibility delegated and it doesn’t develop reflexes.”
The only walker that is generally approved is the stroller with wheels, which the child uses a handlebar to push. “At least they are pushing something. That’s not too bad. They push it like they would something else [a chair, for example] to help them,” says Asso.
Feeding: breast milk or baby formula?
In the first three months of life, a baby gains around 900 grams in weight and 3.5 centimeters in height each month. From four months to six months, they gain half a kilogram and two centimeters every four weeks. That is the average growth rate but every baby, in practice, has their own pace. In the first few days after birth, tiny spoonfuls of milk are enough to satisfy and, as they grow, milk-only feeds will increase in quantity up to six months.
From the scientific point of view, there is no debate: breast milk is the best option for the physical and emotional health of a baby and the mother. “As well as the prevention of cancer in the mother and the metabolic gift to the child in terms of prevention of cardiovascular risk, there are other things that go beyond nutrition,” says Asso. “During lactation, there is a hormonal release on the part of the mother, such as oxytocin, which forms bonds between mother and baby.”

Breastfeeding exclusively is
recommended during the
first six months
Milk ducts
Lobules
During breastfeeding, milk naturally adapts to the baby’s growing needs.
At first it is a concentrated liquid called colostrum that is full of proteins, nutrients and white blood cells that protects babies from infection.
Amount
of milk
Mature
milk
Transitional
milk
Calostrum
Birth
72 hours
2 weeks
6 months
Later it turns more liquid and richer in fat, lactose and carbohydrates.

Breastfeeding exclusively is r
ecommended during the first
six months
Milk ducts
During breastfeeding, milk naturally adapts to the baby’s growing needs.
Lobules
Later it turns more liquid and richer in fat, lactose and carbohydrates.
At first it is a concentrated liquid called colostrum that is full of proteins, nutrients and white blood cells that protects babies from infection.
Amount of milk
Mature
milk
Transitional
milk
Calostrum
72 hours
2 weeks
6 months
Birth

Breastfeeding exclusively is recommended
during the first six months
Milk ducts
During breastfeeding, milk naturally adapts to the baby’s growing needs.
Lobules
At first it is a concentrated liquid called colostrum that is full of proteins, nutrients and white blood cells that protects babies from infection.
Later it turns more liquid and richer in fat, lactose and carbohydrates.
Amount of milk
Mature
milk
Transitional
milk
Calostrum
Birth
72 hours
2 weeks
6 months
Asso acknowledges that baby formula has achieved “a very good nutritional quality,” but there is no substitute for breast milk, which is “a dynamic fluid, which changes constantly and adapts to the necessities of the child.” As an example, Asso notes: “There are changes in the temperature of the nipple so that the sebaceous glands emit more odor so that the child can find the breast.”
In this changing fluid, breast milk in the first 72 hours after birth is called colostrum. “It has a yellowish color because it contains carotenes, a precursor to vitamin A. And it is rich in proteins and immunoglobin A, to protect the newly born child,” says Asso. Furthermore, this milk is delivered in small quantities “because the coordination between sucking and breathing needs to be established.” In the same feed, the first part of the milk is watery, to quell thirst. In the second phase, the milk is more calorific, with a greater fat content to satisfy hunger.
How and when to start complementary feeding
Experts recommend breastfeeding exclusively up to six months and phasing in complementary foodstuffs from there. In the case of children who have not been breastfed, there is no clear consensus, but it can be introduced from between four and six months.
Starting too early (before four months) can be dangerous due to the risk of choking, the substitution of milk for other, less nutritious foods and long-term dysregulation of appetite and satiation. As such, the Spanish Pediatric Association (AEP) recommends not delaying the introduction of other foods beyond 26 weeks as this can lead to nutritional problems such as iron or zinc deficits and food allergies.
Pediatricians recommend introducing other foods gradually, and although AEP guidelines have for many years have broken down bringing in new products month-by-month, pediatricians say they are now much more flexible. For example, previously the more allergy-inducing foods, such as eggs and some kinds of fruit, were introduced last, for fear of children developing intolerances. But scientific evidence did not back that theory. “Postponing allergenic foods was done with the best of intentions, to reduce risks, but it transpired it didn’t make a lot of sense,” says Asso.
What pediatricians do agree on is that when starting to introduce complementary foods, they should be high in iron and zinc content, such as meat, fish and legumes. And, as Coronel notes, always adapting to the needs of the child. “It is not necessary to be categorical or dogmatic. The order in which foods should be introduced is variable; with a heavier child, you can bring in vegetables before cereals, for example.”
The only guidelines the experts stipulate are that vegetables with green leaves (such as spinach and chard) should be avoided until 12 months and that fruit should be given whole (fruit juices have practically no nutritional value). The Spanish Health Ministry also recommends avoiding large fish, such as swordfish and tuna, until the age of 10.
Teething
It is as normal for a child’s first tooth to appear at the age of five months as it is at 12 months. In either case, pediatric dentists recommend that from birth, even when a child has no teeth, cleaning the gums and tongue with a mist gauze after each feed.
After the first teeth come through, dental hygiene can be carried out with silicone thimbles or a small toothbrush, at least twice a day. When the first molars break through, pediatric dentists recommend flossing. Asunción Mendoza, president of the Spanish Society of Pediatric Dentists, suggests brushing for a couple of minutes, using an amount of toothpaste about the size of a grain of rice up until two years and spitting out the toothpaste without rinsing.

Appearance
Central incisor
6-10 months
Lateral incisor
10-16
Canines
17-23
First molar
14-18
Lower
teeth
Second molar
23-31
Central incisor
9-12
Lateral incisor
9-13
Canines
6-22
First molar
13-19
Upper
teeth
Second molar
25-33

Appearance
Central incisor
6-10 months
Lateral incisor
10-16
Canines
17-23
First molar
14-18
Lower
teeth
Second molar
23-31
Central incisor
9-12
Lateral incisor
9-13
Canines
6-22
First molar
13-19
Upper
teeth
Second molar
25-33

Appearance
Appearance
Central incisor
6-10 months
Central incisor
9-12
Lateral incisor
10-16
Lateral incisor
9-13
Canines
17-23
Canines
6-22
First molar
14-18
First molar
13-19
Lower
teeth
Upper
teeth
Second molar
23-31
Second molar
25-33
Dental caries is an infectious disease that is more common in infancy and its advance, because of the properties of milk teeth, is very fast. Pediatric dentists back breast milk as the best option for a baby’s development, and although that alone will not provoke caries, they warn that nighttime breastfeeding over a prolonged period (more than a year), combined with poor post-feeding hygiene, can lead to the development of caries. After the first tooth comes through, bottle-feeding should be avoided at night.
There are other habits, says Mendoza, that can also pose a risk: if one of the parents has a tendency to develop caries, they will have carcinogenic bacteria that can be transmitted by saliva, in actions as common as “cleaning a pacifier with saliva, testing a bottle to see if it is too hot, blowing on food to cool it down, or kissing your baby on the lips; these can all allow the bacteria that produce caries to be passed from the adult’s mouth to the baby’s.”
Baby-led weaning or blended food?
When it comes to how to feed a baby, there are two options: the traditional way, blending food, or so-called baby-led weaning, which consists of introducing foods on the baby’s direction (they eat whatever is on the table and catches their eye). There are no studies to suggest one way is better than the other, so the experts say it is up to the parents to decide which they prefer.
“The baby’s mastication is dependent on gum strength. They cannot cut food, but they can chew. Baby-led weaning is interesting because we foment development and the baby’s independence, and furthermore, as they are eating at the table, it is a moment of incalculable value for the child,” says Asso, who also points out the benefits of “shared responsibility:” the baby eats depending on appetite.
Coronel, however, says “it is a good idea as long as the baby is eating enough and getting enough nutrition.” Care also has to be taken over the risk of choking. Small and tough foods should be avoided, such as nuts, apples and carrots. Experts recommend steamed vegetables or softer fruits cut into small slices, like pears, bananas and mangoes.
The pacifier has its limits
Pediatricians recommend avoiding pacifiers as much as possible, above all when breastfeeding is being introduced and the baby is working out suction and the most comfortable position. Asso points out that pacifiers and baby bottles can create confusion. “Pacifiers are easier to suck on and all of the knowledge and practice a baby is acquiring with breast suction is conflicted by that of the pacifier.”
In any case, if parents decide to use a pacifier, pediatricians say it should only be used at certain times, such as to help the baby to relax to sleep. “But limits must be established because they have an open bite and open arches and this will almost certainly be synonymous with orthodontics,” says Asso.
Socializing: from crying to tantrums
A newborn spends almost all day sleeping, waking up only to eat and communicating through crying. But as the months go by, their contact with their surroundings increases and goes from a small, mimicking smile in the first month when comfortable or satisfied, to paying attention to voices, babbling, playing and wanting to talk and interact with other people.
Between the ages of six months and a year, babies are experts in non-verbal communication. They make themselves understood with gestures, make their preferences known and express their emotions. They enjoy playing and start to understand that toys will continue to exist even if they can’t see them.
Little by little, they gain curiosity, become interested in new things and start to develop their character and personality. As they approach their second birthday, they become more and more independent, capable of hugging, kissing or rejecting someone. They also have tantrums when they don’t get what they want. They recognize themselves in the mirror and start to become aware of themselves in their own right. They also imitate the actions of adults and want to play with other children. Encouraging the development of their brains with games, attention and care also helps to build social skills that will be key in communicating with the world.
Is co-sleeping a good idea?
Sleeping in the same bed is a controversial practice: on the one hand, it makes breastfeeding easier, but it is also a risk factor for SIDS. If parents decide to co-sleep, pediatricians advise following a few guidelines. In the days after birth, for example, when the mother is tired and worn out, the risk of crushing the baby is higher. “But co-sleeping aids attachment and breastfeeding,” notes Victoria Fernández de la Rúa of the AEP, which also states that continuous contact helps to build bonds of affection and is good for the baby’s health and neuronal development. However, the AEP advises that the safest place for babies to sleep in the first six months of life is in a crib, face up and close to the parents’ bed.
While co-sleeping facilitates breastfeeding, which is a protective factor against SIDS, the practice itself poses a risk. As such, experts recommend not co-sleeping with babies who are less than three months old, with premature babies or those who were underweight when born, if the parents smoke, drink alcohol or take drugs or pharmaceutical sedatives, or in situations of extreme tiredness. They also advise against co-sleeping on soft surfaces, such as water beds or couches.
Screen-time: when and how much?
Screens should be avoided in their entirety until the age of two. On this, pediatricians are unanimous. “Children should not be calmed in this way or distracted so that they eat. Screens affect their sleep and encourage sedentarism and obesity,” says Fernández de la Rúa.
Asso goes even further and says screens can also affect the relationship between children and parents. “When you are looking at your cellphone, it interferes with your life and your relationships with everyone else. Screens can hold us hostage.” Specifically, putting a screen in front of a child when they are eating can lead to “the child eating without being aware that they are eating, and this may cause them to skip appetite and satiety cues because they are eating on auto-pilot.”
Should you let your baby cry?
Babies can cry for between one and three hours a day during the first three months of life, without any significant pathology. It is the way they communicate their needs. They cry when they are cold, when they are hot, when they are hungry, if they feel alone or simply because they want to play.
Pediatricians advise “common sense” when it comes to dealing with this situation. Firstly, any possibility of health problems should be ruled out, or any discomfort. If this does not apply, parents should attempt to console the child and break the cycle of crying by moving the baby to another room to look through a window or to play a game, for example. “When a baby cries they are transmitting a need. You have to go. Then, deciding whether to console them by picking them up or not depends on each case,” says Asso.
Warning signs: when something is not right in development
Pediatricians advise caution and underline that every child is different and has their own particular rhythm of development. Comparisons, with brothers and sisters at home or friends at nursery or in the park, are of little value, they emphasize. Beyond the personal perception of parents or the opinion of peers, professionals monitor the psychomotor development of children through scientifically validated scales, such as the Haizea-Llevant scale, a development table that calculates parameters of sociability, manipulation, language and posture on a month-by-month basis.

Developmental warning signs
2 months
Excessively
jumpy
Permanently
irritable
Expressive
passivity
Asymmetry
of hands
Persistently
jumpy
Abnormal
increase
in muscle tone
Repetitive
behavioral
pattern
Cannot move
around
autonomously
12
No longer
babbles
Transitioning
from one
activity to
the next
without pause
Verbal
repetition
Inability to
develop
symbolic play
24

Developmental warning signs
2 months
12
24
36
Socializing
Permanently irritable
Transitioning from one activity
to the next without pause
Excessively
jumpy
Repetitive behavioral
pattern
Inability to develop
symbolic play
Persistently jumpy
Lenguage
Express passivity
No longer babbles
Verbal repetition
Posture and grasping
Adduction
Cannot move around
autonomously
Asymmetry of hands
Abnormal increase in muscle tone

Developmental warning signs
2 months
12
24
36
Socializing
Permanently irritable
Transitioning from one activity to the
next without pause
Excessively
jumpy
Repetitive behavioral
pattern
Inability to develop symbolic play
Persistently jumpy
Lenguage
Express passivity
No longer babbles
Verbal repetition
Posture and grasping
Adduction
Cannot move around
autonomously
Asymmetry of hands
Abnormal increase in muscle tone
Sources: Spanish Association of Pediatrics, Spanish Society of Pediatric Dentistry, Andalusian Association of Primary Care Pediatrics, Spanish Society of Pediatric Neurology, Spanish Society of Outpatient Pediatrics Primary, Department of Health of the Generalitat of Catalonia, World Health Organization.