Monkeypox is down, but US cities could be at risk for summertime outbreaks
A bigger supply of vaccines, more people with immunity and readier access to treatment point to fewer and less severe infections, but a false sense of security still poses a risk
The monkeypox health emergency has ended, but U.S. health officials are aiming to prevent a repeat of last year’s outbreaks.
Monkeypox infections exploded early in the summer of 2022 in the wake of Pride gatherings. More than 30,000 U.S. cases were reported last year, most of them spread during sexual contact between gay and bisexual men. About 40 people died.
With Pride events planned across the country in the coming weeks, health officials and event organizers say they are optimistic that this year infections will be fewer and less severe. A bigger supply of vaccine, more people with immunity and readier access to a drug to treat monkeypox are among the reasons.
But they also worry that people may think of monkeypox as last year’s problem.
“Out of sight, out of mind,” said Dr. Demetre Daskalakis, who is advising the White House on its monkeypox response. “But we are beating the drum.”
Last week, the Centers for Disease Control and Prevention issued a health alert to U.S. doctors to watch for new cases. On Thursday, the agency published a modeling study that estimated the likelihood of monkeypox resurgence in 50 counties that have been the focus of a government campaign to control sexually transmitted diseases.
The study concluded that 10 of the counties had a 50% chance or higher of monkeypox outbreaks this year. The calculation was based largely on how many people were considered at high risk for infection and what fraction of them had some immunity through vaccination or previous infection.
At the top of the list are Jacksonville, Florida; Memphis, Tennessee; and Cincinnati — cities where 10% or fewer of the people at highest risk were estimated to have immunity. Another 25 counties have low or medium immunity levels that put then at a higher risk for outbreaks.
The study had a range of limitations, including that scientists don’t know how long immunity from vaccination or prior infections lasts.
So why do the study? To warn people, said Dr. Chris Braden, who heads the CDC’s monkeypox response.
“This is something that is important for jurisdictions to promote prevention of monkeypox, and for the population to take note — and take care of themselves. That’s why we’re doing this,” he said.
Officials are trying to bring a sense of urgency to a health threat that was seen as a burgeoning crisis last summer but faded away by the end of the year.
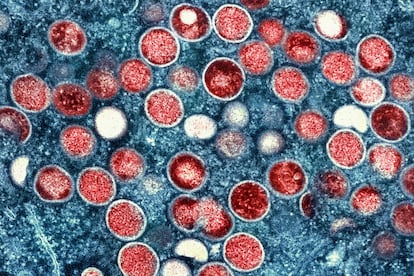
Monkeypox is caused by a virus in the same family as the one that causes smallpox. It is endemic in parts of Africa, where people have been infected through bites from rodents or small animals, but was not known to spread easily among people.
Cases began emerging in Europe and the U.S. about a year ago, mostly among men who have sex with men, and escalated in dozens of countries in June and July. The infections were rarely fatal, but many people suffered painful skin lesions for weeks.
Countries scrambled to find a vaccine or other countermeasures. In late July, the World Health Organization declared a health emergency. The U.S. followed with its own in early August.
But then cases began to fall, from an average of nearly 500 a day in August to fewer than 10 by late December. Experts attributed the decline to several factors, including government measures to overcome a vaccine shortage and efforts in the gay and bisexual community to spread warnings and limit sexual encounters.
The U.S. emergency ended in late January, and the WHO ended its declaration earlier this month.
Indeed, there is a lower sense of urgency about monkeypox than last year, said Dan Dimant, a spokesman for NYC Pride. The organization anticipates fewer messages about the threat at its events next month, though plans could change if the situation worsens.
There were long lines to get shots during the height of the crisis last year, but demand faded as cases declined. The government estimates that 1.7 million people — mostly men who have sex with men — are at high risk for monkeypox infection, but only about 400,000 have gotten the recommended two doses of the vaccine.
“We’re definitely not where we need to be,” Daskalakis said, during an interview last week at an STD conference in New Orleans.
Some see possible storm clouds on the horizon.
Cases emerged this year in some European countries and South Korea. On Thursday, U.K. officials said an uptick in monkeypox cases in London in the last month showed that the virus was not going away.
Nearly 30 people, many of them fully vaccinated, were infected in a recent Chicago outbreak. (As with COVID-19 and flu shot, vaccinated people can still get monkeypox, but they likely will have milder symptoms, officials say.)
Dr. Joseph Cherabie, associate medical director of the St. Louis County Sexual Health Clinic, said people from the area travel to Chicago for events, so outbreaks there can have ripple effects elsewhere.
“We are several weeks behind Chicago. Chicago is usually our bellwether,” Cherabie said.
Chicago health officials are taking steps to prevent further spread at an “International Mr. Leather” gathering this weekend.
Event organizers are prominently advising attendees to get vaccinated. Chicago health officials put together social media messages, including one depicting three candles and a leather paddle that reads: “Before you play with leather or wax get yourself the monkeypox vax.”
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.








































