Endometriosis: Science begins to unravel the mystery of a disease affecting millions of women
The study of infections and genetic analysis are seeking new solutions to a condition that until recently was largely ignored

Up to 10% of women suffer from endometriosis, and yet this disease is still shrouded in mystery. “It is as if we were making a jigsaw puzzle, we are collecting pieces, but we don’t know what image we are looking for, we don’t have a model that makes sense of it all,” explains Francisco Carmona, head of the Gynecology Service at Hospital Clínic in Barcelona. After treating this ailment with surgery or hormonal treatments for decades, specialists like Carmona believe that in the coming years, our understanding of the genetic causes of the disease and the integration of data made possible by artificial intelligence may offer new alternatives to patients, as well as a theory that will help to understand what we are trying to cure.
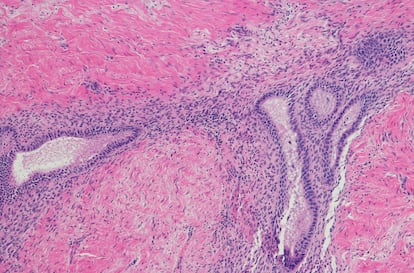
This disease occurs when the endometrial tissue, which covers the inner part of the uterus and serves to house an embryo, grows where it should not. This tissue responds to the sexual hormones produced by the ovaries, and once a month it thickens, preparing the woman for a possible pregnancy. The thickened and misplaced endometrium, in the ovaries, pelvis and even beyond, causes the pain that many women associate with menstruation. It can also make sexual intercourse or simply urinating painful, and it is behind many cases of infertility.
“Until not so long ago, period pain was trivialized by doctors, as well as women who, many times, in an ailment with a hereditary component, had their mother as a reference point who told them that this pain was normal. This would delay diagnosis and treatment for years,” says Estela Lorenzo, a specialist at the Endometriosis Unit of Hospital 12 de Octubre in Madrid. “That has changed, especially for women. Doctors are taking much more interest because women are becoming more demanding, they do not accept that period pain is normal, they demand to know the cause of their pain and a treatment, and they do not allow themselves to be treated with condescension,” agrees Carmona.
However, Lorenzo adds, it will take more than a change in perception and attitude. “We don’t have tests that allow us to detect the disease in its early stages. When we do an ultrasound, despite the fact that they have improved a lot, we may not see anything in a woman who is in pain. Now, in France, there is an approved saliva diagnostic test that allows early detection. This type of minimally invasive and rapid tests is necessary,” explains Lorenzo, who also believes that the paradigm shift of recent years is going to change the treatment of endometriosis. “Previously it was seen as a gynecologic disease only, which is first local or pelvic, but now it is seen to have a systemic inflammatory component,” she adds.
A few days ago, the journal Science Translational Medicine published a study by researchers from the University of Nagoya (Japan) that claimed that the presence of a type of bacteria could be behind some cases of endometriosis. In the study, 155 women were analyzed, 79 of them with endometriosis and the rest without. In 64% of the former, an infiltration of Fusobacterium, a type of microorganism that causes, among other things, periodontal diseases, was identified. Among the healthy volunteers, the figure was less than 10%. According to the researchers, these bacteria could be behind the increase in transgrelin, an endometriosis-associated protein that could overgrow due to the presence of a growth factor generated as part of the immune system’s response to infection. This mechanism was then tested in mice inoculated with Fusobacterium that caused the increase in transgrelin and endometriosis-associated lesions. The scientists then gave the animals antibiotics to eliminate the infection. With it, the endometriosis problem was also reduced, something that, according to those responsible for the study, opens the door to using antibiotics as an alternative treatment to hormones in women with endometriosis.
“These results were very surprising, because we have treated many women with antibiotics, and they have not improved. It is one more piece of the puzzle, it is provocative and interesting, but I would be cautious before concluding that antibiotics can be used to treat endometriosis,” says Carmona. Estela Lorenzo also raises the difficulty of establishing cause and effect and recalls the anatomical differences between mice (which, among other things, do not menstruate) and humans. However, she recognizes the importance of work like this in identifying the link between the triggers of chronic inflammation, such as bacteria, and the origin of endometriosis. “It is possible that there are some patients who are genetically predisposed and who initiate this inflammation by fusobacteria. There are many studies on the role of the microbiome in this disease, and we have examples of ailments such as ulcers, which were associated with stress before Helicobacter pylori was identified as the cause, or human papillomavirus and cervical cancer,” explains Lorenzo. Carmona has more faith that clinical solutions to the disease “will come through knowledge of genetics than through antibiotics.” This year, a collaboration of 25 scientific teams from around the world published the largest study to date on the genetics of endometriosis. Analysis of the DNA of 60,600 women with endometriosis and 701,900 who did not have it revealed, for example, a shared basis between this ailment and other apparently unrelated painful experiences such as migraine or back pain. This is consistent with the specialists’ observation that sometimes a woman may suffer a lot of pain that does not correspond to the lesions seen on imaging.
The authors of the paper, which was published in Nature Genetics, propose that genetic predisposition may cause endometriosis to initiate inflammatory mechanisms that lead to excessive sensitization of the central nervous system. This would cause pain to be felt more intensely in different parts of the body that have nothing to do with the initial endometriosis. Something that shows the complexity of this disease is that, in addition, the pain in places far from the uterus that recurs with menstruation may be the result of tissue implants at a distance, which, like a tumor cell, migrate from one organ to another. “Implants have been described in peripheral organs such as the sciatic nerve or pneumothorax associated with menstruation, which are indeed due to a direct implant of endometriosis,” Lorenzo points out.
Carmona says he has received an invitation to participate in an international project to search for imaginative approaches to overcome the stagnation of the last 40 years in research into the origin of the disease and to include new treatments. This initiative for endometriosis suggests that the lack of new solutions is due to the fact that almost all lines of work start from the same hypothesis. In this search for alternative hypotheses, Carmona states: “There are combinations of genes that increase the risk of endometriosis, and detecting them in time would make it possible to avoid reaching more serious stages. We can consider testing gene therapies if we discover that certain genes play a preponderant role in the development of the disease, or adopt preventive or therapeutic strategies if we detect interactions between genetic factors and infections or in combination with specific types of environmental pollution that trigger the disease,” he adds.
Going back to the analogy of the puzzle, Carmona states that pieces continue to be found and that soon, perhaps not soon enough for women suffering from the disease today, but very quickly in scientific terms, theories will emerge that will change our understanding of endometriosis and its treatment. “There is a combination of causes, genetic, epigenetic, environmental. We know that women who are born premature have a higher risk of endometriosis than those of normal weight, that women who were breast-fed have less risk, that there is a greater anatomical endometriosis in women who suffered abuse, either physical or psychological, and we are also making progress in molecular tools to correct defects in hormone receptors associated with the disease. We have to put many pieces together, we do not even have a model yet, but I am hopeful,” he concludes.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































