A personalized vaccine could aid in the fight against pancreatic cancer, the deadliest form of the disease
Eight patients responded positively to an experimental treatment that combined a vaccine using mRNA tailored to each patient’s tumor and conventional drugs
Of the more than 100 known types of cancer, pancreatic cancer is the most lethal. 88% of patients who have this type of cancer die despite having received the available treatments, which mostly involve surgery and chemotherapy. However, this terrible statistic has a bright side: 12% of the patients survive. Some live for years, even more than a decade, without the cancer coming back. In medical terms, they are cured. How do they do it?
This question has inspired the development of a vaccine against pancreatic cancer based on messenger RNA, the same molecule that made it possible to create immunizations against Covid-19 in record time. The results of the first tests on patients — just 16 people in a first round of trials — have shown promising results. The vaccine has succeeded in activating the immune system in half of the patients. None of them relapsed during the 18-month trial period. On the other hand, all the patients in whom the vaccine did not provoke a reaction suffered relapses.
The results are still very preliminary, but they mark an important milestone in a field in which treatments and patient survival have hardly improved in the last 40 years.
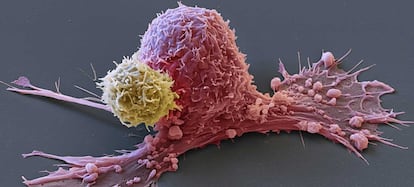
Pancreatic cancer is the quintessential cold tumor. In oncological jargon, a cold tumor refers to one that is not likely to trigger a strong immune response. Therefore, the immune system is incapable of detecting it and provoking inflammation — heat — to kill it. This is why immunotherapy, the most successful cancer treatment in recent years, does not work in the pancreas. What is surprising is that the tumors of long-term survivors of pancreatic cancer are burning up: there are up to 12 times more immune cells in them than in other patients. These immune cells are killer T-lymphocytes, a type of white blood cell capable of killing other cells. The survivors’ T cells have learned to identify the aberrant proteins produced by the tumor — called neoantigens — and kill it.
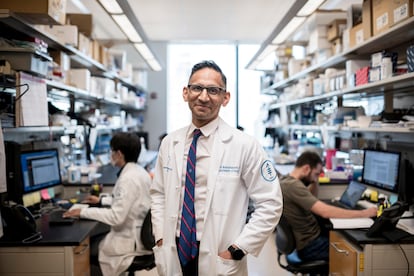
“After analyzing samples from long-term survivors, we asked ourselves whether we could emulate this in the rest of the patients,” Vinod Balachandran, a physician at the Sloan Kettering Cancer Center in New York and leader of the team that developed the vaccine, explained to EL PAÍS. The most important thing, he added, is that, contrary to what was thought until now, pancreatic cancer does produce molecules that allow the immune system to be launched against it.
The results are published this Wednesday in the journal Nature. Ugur Sahin and Özlem Türeci, the now famous Turkish-born couple who founded BioNTech and created the successful mRNA vaccine against Covid in collaboration with Pfizer, also worked on the investigation. The fact is that the two researchers set up their company precisely with the idea of creating the first effective vaccines against cancer.
In this clinical trial, a vaccine had to be manufactured for each patient. After removing the tumors from the abdomen of the 16 participants, the researchers sequenced their genomes and identified up to 20 neoantigens. They then created the vaccines containing the recipe for each to synthesize the tumor-specific molecules in their bodies.
The patients were given atezolizumab, an immunotherapy drug, a dose of the vaccine and finally mFolfirinox, a type of chemotherapy. They then got a booster dose. In addition to the positive results in the aforementioned 50% of patients, the researchers observed an increase in the number of killer lymphocytes in their bodies, which is probably behind the absence of relapses. Balachandran explained that they hope to start “soon,” together with BionTech, a second phase of more detailed tests with more patients, which is essential to ascertain the real effectiveness of the vaccine.
“These results are very promising and lay the groundwork for a second phase of clinical trials,” emphasized Amanda Huff and Neeha Zaidi, researchers at Johns Hopkins University who were not involved in the study. These oncology vaccine specialists also highlighted a surprising observation. One of the patients who responded to the vaccine had killer lymphocytes not only in his pancreas, but also in his apparently healthy liver. Why? Apparently he had a non-cancerous lesion characterized by a mutation in the TP53 gene, which is the same as the one in his pancreatic cancer. This suggests that the immune system activated by the vaccine could fight not only the primary tumor, but also metastasis in other organs.
“A survival time of 18 months without relapse is a very respectable”Ignacio Melero, University Clinic of Navarra (Spain)
Ignacio Melero, an expert in immunotherapy at the University Clinic of Navarra (Spain), praised the results of the study: “When the surgeon removes these tumors there is usually residual disease. These results show us that it may make sense to add this vaccine, which is the first mRNA vaccine to show positive results in the pancreas, to conventional treatments. A survival time of 18 months without relapse is a very respectable.” But the oncologist also warned that, for now, “the technology to develop these vaccines is very complex, especially because you have to make one vaccine per patient.”
Ana Fernández-Montes, spokeswoman for the Spanish Society of Medical Oncology, believes that this is a “very hopeful approach.” “We are talking about a tumor that after surgery can only receive chemotherapy to avoid relapses, a treatment that has a high failure rate and with very significant toxicity,” she said. “We are converting a cold tumor, which does not respond to immunotherapy, into a hot tumor, which potentially will [respond to treatment],” she added.
Balachandran spoke about the limitations of his work. “It’s hard to compare what we see in vaccinated patients with what we saw in long-term survivors, but we do know that the type of immune cells that are activated are the same: CD8+ killer T lymphocytes,” he explained. The doctor says that this experimental vaccine needs to be studied further by slightly modifying the combination times with chemo and immunotherapy to see if it improves effectiveness. They will also have to answer the most pressing question: why did only half of the patients react to the vaccine?
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































