The dream of a universal cancer vaccine… we’re getting closer
Results from animal experiments reveal a revolutionary method that stimulates the immune system to destroy even the most resistant tumors
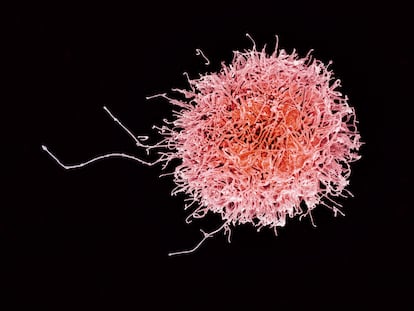
In recent years, the forefront of cancer research has focused, not on the inside of the tumor, but on everything that surrounds it. Oncologists call this the microenvironment: a microscopic world that is still poorly understood. Tumor cells advance by latching on to new blood vessels, which feed their peculiar growth. In many cases, bacteria build up around the tumor which can be responsible for aggravating the disease. In some instances, there are also immune system cells that seem to be asleep. In the environment of the most lethal and difficult to treat tumors - such as those of the pancreas or brain - there are very few T lymphocytes, the immune cell capable of locating and eradicating any external threat. It’s as though cancer were wearing an invisibility cloak. Nine out of ten cancer deaths are due in part to this issue: when doctors detect the disease, it has already spread to other organs causing metastasis.
One of the biggest challenges in oncology is to create vaccines that bring different forces from the immune system to the battlefield of the tumor microenvironment, regardless of the affected organ. For this reason, a molecular mechanism common to all tumors must be found. What complicates the matter is that cancer has been evolving alongside us for millions of years and uses biological mechanisms very similar to those of healthy cells. Killing it can also mean killing the patient. This difficulty has meant that most cancer vaccines currently being pursued are personalized for each patient and their cancer. This poses enormous economic and technical challenges: cancer is one of the most prevalent diseases in the world with some 18 million new cases diagnosed each year.
A new study has revived the dream of a polyvalent cancer vaccine. This involves a new molecule identified by physician and immunotherapy expert Kai Wucherpfennig from the Dana-Farber Cancer Institute in Boston that uses a different tactic to remove tumors’ invisibility.
Cancer damages the DNA of cells, and in response to that damage, two proteins called MICA and MICB are produced. Under normal conditions they would serve to alert the immune system, but cancer has developed the ability to cut and dilute them, making it invisible to the body’s defenses.
David Mooney’s team, a bioengineer at Harvard University, designed a vaccine based on the molecule identified by his colleague at Dana-Farber that generates antibodies against these two proteins. These molecules bind to them and prevent them from being cut. That removes the tumor’s invisibility cloak and brings two types of immune cells to the site: T cells and natural killer cells. Both are again able to identify the proteins, bind to them and destroy tumor cells where they are present.
Scientists have demonstrated that the vaccine is effective, with successful results from experiments in mice and they have also observed that an adequate immune response is produced in monkeys. This immunization remains even in cases of advanced tumors that have metastasized in animals.
“This vaccine could help many patients with different types of cancer because it does not depend on the specific mutations in each patient’s cancer,” explains bioengineer Mooney.
His team has spent years developing vaccines based on three-dimensional microscopic structures that, once injected, function as a headquarters to which tens of thousands of cells of the immune system flock, capable of generating antibodies against tumor proteins and stimulating other effective ones, especially T lymphocytes and the natural killers.
This new cancer vaccine prototype has been published in Nature, a leading reference in world science. One of its most outstanding characteristics is that it disables one of the invisibility mechanisms of the immune system most used by tumors, including those of the pancreas and brain glioblastoma. “The main message is that it is possible to develop vaccines that work in many patients and in different types of tumors”, summarizes Wucherpfennig. The team plans to start clinical trials with patients next year.
The development of effective drugs against cancer is an arduous undertaking. Only three of every 100 new drugs of this type manage to pass all clinical trials and reach the market. The success rate is even lower in the fight against more complicated tumors. However, along with other approaches, this vaccine aims to act as a new weapon in combatting cancer, along with already approved treatments.
“This study is part of a new approach to immunotherapy,” explains Ignacio Melero, an immunologist at the University of Navarra’s Center for Applied Medicine Research, in northern Spain. “The idea is to immunize so that autoantibodies are formed against mechanisms used by the tumor to evade the response of the immune system, so that in vaccinated patients the effectiveness of immunotherapy treatments is enhanced. A similar approach with another type of vaccine has achieved promising results against melanoma”, highlights Melero.
This refers to the first clinical trials in patients with an experimental vaccine based on a small protein called IO103 that stimulates the reaction capacity of T lymphocytes and that is administered together with checkpoint inhibitors, a type of immunotherapy against cancer that is already approved. “We have to wait to see the findings from clinical trials, but the results so far suggest that they are up to the challenge,” adds Melero.
Pedro Romero, co-director of the Ludwig Institute for Cancer Research, in Switzerland, summarizes the difficulty of developing non-personalized vaccines. “Cancer is not a uniform disease entity; there may be more than 700 different cancers that are defined by distinctive molecular profiles. All effective anticancer treatments are successful only against a limited number of these cancer subtypes. Nothing different can be expected from future cancer vaccines. It’s possible that some immunizations like the one discovered by the Dana-Farber group could work against a significant group of tumors, which would be an important achievement. The biomarker in this case would be the level of the MICA and MICB molecules in the blood”, he details.
Romero is optimistic about the potential of these therapeutic vaccines. “It is conceivable to use a combination of the two types of vaccines, semi-universal and personalized. There would be potentially beneficial synergies for the treatment of patients. Cancer immunotherapy is in its infancy, reaching adolescence. The expectations are high”, he concludes.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































