Human mini-organs created from fetal cells can treat diseases before birth
European scientists recreate the lungs, intestines and kidneys of fetuses without affecting their growth
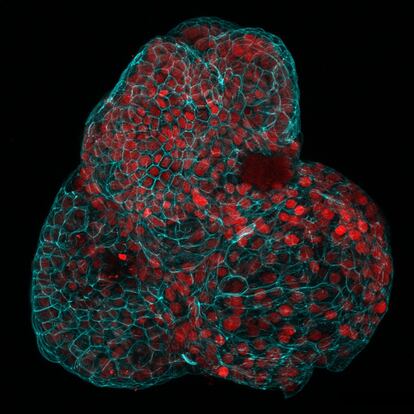
Tissue clusters smaller than a pinhead are the first human fetal mini-organs to be obtained without causing any harm to the future baby or its mother. These three-dimensional copies of the intestine, kidneys and lungs of the fetus open up the possibility of diagnosing and treating congenital diseases before birth and studying stages of human development that are difficult to access through other techniques.
“Until now, there was no way to create organoids in active pregnancies, [it was possible] only if there was an abortion,” explains Mattia Gerli, a biotechnologist at University College London and the lead author of a study involving 27 scientists and physicians from the United Kingdom, Italy and Belgium, published today in Nature Medicine.
Organoids were invented at the end of the last decade. They start as a single microscopic stem cell that multiplies in a petri dish to form miniature intestines, hearts, brains.... One of their most promising experimental uses is reproducing a patient’s organs in order to choose the most appropriate treatment for his/her genetic profile and that of his/her disease, especially in cancer cases. Until now, mini-organs have been made from stem cells extracted from non-viable embryos or reprogrammed adult cells; never before had they been taken from living fetuses developing in utero.
Gerli’s team has achieved this by using the amniotic fluid that envelops the fetus within the mother’s womb. Researchers analyzed samples of this fluid from 12 pregnant women who underwent amniocentesis, a prenatal diagnostic technique. Molecular analysis of this fluid identified epithelial stem cells that had detached from the fetus and are responsible for forming different organs. Cultivated in the laboratory, each of these cells began to multiply and grow to form functional mini-kidneys, mini-intestines and mini-lungs up to one millimeter in diameter. The whole process takes just four weeks. The result is these little cell clusters emulate a fetus’s growing organs in real time.
Researchers have demonstrated this technique’s potential by generating mini-lungs from babies with chronic diaphragmatic hernia. This rare condition causes the intestines and liver to crowd the lungs and impede fetal development. Researchers have shown that these replicas reproduce the molecular features of the disease. The idea is to use the organoids as a diagnostic tool before it is too late to operate on the fetus and choose the best drug treatment among those available.
“We hope that our work will open up new possibilities in prenatal medicine,” says Gerli. The researcher says that the techniques for creating these organs are not complex or expensive, and he advocates creating amniotic fluid stem cell banks, since every year thousands of mothers undergo this diagnostic technique.
In October, an Israeli research team published a preliminary study in which they also generated mini-kidneys and mini-lungs from amniotic fluid stem cells and applied them to the study of two life-threatening congenital diseases. The team noted that eight out of ten birth defects have no known cause. Mini-organs modeled from amniotic fluid may help change that terrible statistic. Moreover, they add, these organoids can be a powerful tool for studying the effects of toxic compounds present in the environment on human development.
The tiny organs created by this team reproduce the state of the fetus’s organs at four to eight and a half months of gestation. That opens up the unprecedented possibility of studying development at very advanced stages without endangering the health of the fetus or the mother.
Biologist Nuria Montserrat, a researcher at the Catalonia Institute for Bioengineering, emphasizes the work’s importance. “It has opened up a new field by using a new type of cell to create organoids,” she says. Organoids make it possible to perform rapid and difficult experiments by other means, such as looking at the coronavirus’ entry into human cells. Recently, they have also made it possible to identify the cells responsible for metastasis in colon cancer. “It no longer sounds so strange to use organoids in research and medicine,” summarizes Montserrat. She coordinates the Biomodels and Biobanks platform, which generated over one million samples in 2022. “Looking to the future, the creation of amniotic fluid biobanks for precise medical treatments of rare congenital diseases is very interesting,” although “in the case of mini-kidneys, they are not as complex as those generated through previous techniques,” she adds.
Spanish biologist Marta Shahbazi heads her own research group on human embryonic development at Cambridge’s Laboratory of Molecular Biology (United Kingdom). She appreciates that this study represents a step toward applying personalized medicine before birth.
Amniocentesis is usually performed between 14 and 22 weeks of pregnancy and requires the use of a long needle that passes through the abdomen and into the mother’s uterus. Although the technique is highly perfected, the risk of losing the baby is up to one in every 100 pregnancies. For that reason, it is only used as a method for confirming possible deformities or genetic disorders previously detected through non-invasive tests. Once the amniotic fluid has been analyzed, it is usually discarded. Shahbazi emphasizes that this study is “highly valuable” because it recovers that precious biological material and explores its medical potential without requiring the mother to undergo additional tests.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































