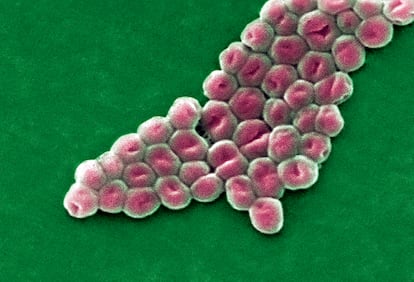
The invisible threat of superbacteria
Antibiotic resistance is on the rise, prompting scientists to emphasize prevention and responsible medication use
There is an unseen threat that keeps the planet on edge. Alexander Fleming warned about it long before it materialized. Eight decades ago, in a prophetic speech after receiving the Nobel Prize in Medicine for his discovery of penicillin, Fleming cautioned: “The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant.” Fleming’s omen proved true. Today, a global epidemic of bacterial resistance spreads freely, causing deaths from once curable infections.
Bacterial resistance currently kills about 1.2 million people worldwide, and experts predict this number will increase tenfold by 2050. “We’re in a critical situation that requires everyone’s cooperation to halt this pandemic. Some patients receive state-of-the-art antibiotics but still succumb due to their ineffectiveness. And this isn’t going to ease up,” warns microbiologist Bruno González-Zorn, director of the Antimicrobial Resistance Unit at the Complutense University of Madrid and an advisor to the World Health Organization (WHO). In Spain, a study across 130 hospitals found that multi-resistant bacteria cause 20 times more fatalities than car accidents. In 2023, over 23,300 deaths were attributed to antibiotic-resistant infections.
This superbacteria species is garnering attention and concern from public health officials. Experts emphasize the need for a dramatic change in direction to reverse dire projections in the short and medium term. “Globalization of antibiotic-resistant bacteria is on the rise. They were once limited to attacking immunosuppressed patients in hospitals, but now they have made their way into the community, causing tuberculosis and sexually transmitted infections,” said María del Mar Tomás, a researcher at the Biomedical Research Institute of A Coruña and spokesperson for the Spanish Society of Infectious Diseases and Clinical Microbiology.
The misuse and abuse of antibiotics, both in healthcare and veterinary settings, are contributing to the growing health crisis. This problem is exacerbated by other factors like the lack of new antibiotics and climate change, which favor the persistence of multi-resistant bacteria. Additionally, the Covid-19 pandemic has led to increased antibiotic consumption in hospitals to treat secondary bacterial infections in coronavirus patients.
González-Zorn says bacteria are remarkable organisms with an incredible ability to adapt. They possess the means to mutate their genetic information, allowing them to overcome challenges like antibiotics and colonize new environments. They can not only multiply with resistance but also transfer it to other bacteria. González-Zorn notes that no one is safe from these microbes. “Even individuals who do not take antibiotics are still susceptible. The impact of bacteria extends beyond the person taking antibiotics and affects us all.”
Globalization also spreads resistance. For instance, when someone travel to India, where superbacteria are prevalent, they often return as carriers of multi-resistant strains. “While they may not have any immediate symptoms, if they contract an infection, it becomes harder to treat. Additionally, they can spread the bacteria to others around them,” said Jordi Vila, a microbiologist and director of the Antimicrobial Resistance Initiative at the Barcelona Institute for Global Health. González-Zorn says that the establishment of multi-resistant bacteria in a country depends on local antibiotic consumption. “Bacteria that are resistant to antibiotics have a significant advantage when the drug is present in the environment. Conversely, sensitive bacteria flourish when the antibiotic is absent from the environment.”
The WHO closely monitors a few of these tiny adversaries, which are extremely dangerous and urgently require new antibiotics. “Acinetobacter baumannii remains the leading concern because we’ve identified some pan-resistant strains of this bacterium,” said Vila. Pan-resistant bacteria are able to overcome every available antibiotic.
And these are not isolated cases, says González-Zorn. “We are increasingly confronted with the reality that we can no longer rely on antibiotics as a cure for some patients.” This means that there are no therapeutic alternatives for certain people. “When an infection affects a body part, amputation is sometimes necessary to eliminate it. It may sound primitive, but it’s the appropriate course of action. In other cases, medical support is provided to patients in order to enhance their immune systems and help them fight the infection.”
In response to this grave situation, public health officials and scientists are collaborating on the One Health strategy, which uses multiple approaches to address the problem. “Resistant bacteria leave hospitals and can be found in pets and wastewater. Therefore, we must combat them both within and outside the hospital,” said González-Zorn. Countries are reducing antibiotic use in veterinary settings and rationalizing healthcare to prevent new superbacteria. Antibiotic disappearance from the environment can even restore sensitivity in some bacteria. But there is still a long way to go. “We may witness a decrease in resistance slope, but zero resistance is unattainable. It will continue to increase, albeit at lower levels. New antibiotics are crucial,” said Vila.
New antibiotics aren’t expected soon. Experts acknowledge that the pharmaceutical industry doesn’t see the development of these drugs as profitable. They suggest introducing economic incentives to reignite interest. Meanwhile, they are exploring other avenues for finding therapeutic tools, such as phage therapy — viruses that can eliminate bacteria and have been tested for certain infections. “Natural phages can be used alongside antibiotics to treat infections. If natural phages are not found, genetically designed or synthetic phages can be created,” said Tomás.
Prevention is crucial, says González-Zorn, who emphasizes the need for further improvement in this area. “In Spain, there is a higher rate of self-medication compared to the rest of Europe. Approximately 5% of pharmacies provide antibiotics without prescriptions. It is crucial to prescribe antibiotics responsibly, not only to treat patients but also to preserve the efficacy of modern antibiotics for future use. Increasing awareness and involvement is necessary.” He states that the progression of this health crisis will largely rely on global improvements, but the situation remains uncertain. “A pan-resistant bacterium could spread rapidly and cause high mortality, but I don’t think that will happen. I believe it’ll just continue to be a silent pandemic, slowly progressing over time.”
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































