Experimental treatment in Spain puts 18 cancer patients in complete remission
Barcelona’s Clínic Hospital announces hopeful results for people with multiple myeloma. Developed through the public system, the cost is lower than commercially available products

When Joan Gel uses the word “here,” he means the land of the living. “In other countries, and I’m not even talking about the Third World, I wouldn’t be here anymore,” says Gel, 67, a resident of Mataró (Barcelona) who used to work at a detergent factory. Now retired, he believes he owes his life to Spain’s public healthcare system.
Twelve years ago, Gel was diagnosed with multiple myeloma, the second most common type of blood cancer. He tried all available treatments but they failed one after the other, from chemotherapy to a bone marrow transplant.
Then, a year and a half ago, Barcelona’s Clínic Hospital offered him the possibility to try an experimental therapy called ARI-0002h. He said yes.
One of his doctors, the hematologist Carlos Fernández de Larrea, on Friday announced at a news conference that Gel is in “complete remission.” And he is not the only one: 18 out of the 30 patients who participated in the trial treatment showed no evidence of disease, representing a complete remission rate of 60%.
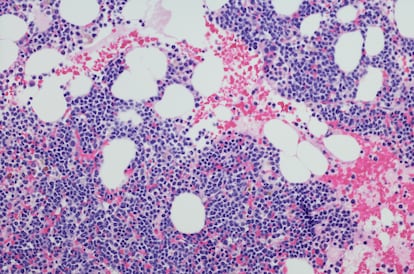
Multiple myeloma is an incurable cancer found in the bone marrow, which normally contains immature cells that transform into new blood cells – red blood cells, white blood cells and platelets. Multiple myeloma causes abnormal growth of plasma cells, a type of white blood cell that produces antibodies, the first line of defense against infection. The survival rate after five years is around 50%.
Even though it is an incurable disease, achieving complete remission has a significant impact on patient prognosisFernández de Larrea, hematologist
The new therapy extracts blood from the patients, selects their T cells (another type of white blood cell) and redesigns them in the lab through genetic engineering, making them better able to recognize cancer cells.
Joan Gel still remembers the day that hospital staff walked into his room with the treatment. It was in the summer of 2020, with the hospital immersed in strict Covid-19 isolation measures. “They finished defrosting it in the room, in a bain-marie with nice hot water. It’s kind of like cooking,” he said at the news conference. Once back into his body, the re-engineered T cells identified the cancer cells and eliminated them.
Complete remission does not mean cured, but it does mean that all signs of the disease are gone. “Even though it is an incurable disease, achieving complete remission has a significant impact on patient prognosis. It is directly linked to greater survival,” said Fernández de Larrea.
For Joan Gel, ARI-0002h was his fifth and most desperate attempt at beating back cancer. Complete remission is more likely to happen in the earlier attempts, for instance with a bone marrow transplant. After that, the probability of achieving remission becomes “very, very low” according to Fernández de Larrea.
ARI-0002h belongs to a new generation of treatment known as CAR-T, or chimeric antigen receptor T cells, which are engineered to produce special receptors. This kind of treatment has become the great hope for many tumors ranging from certain lymphomas to leukemia.
There are two commercial therapies already available, made by the pharmaceutical companies Bristol Myers Squibb and Janssen, but Fernández de Larrea noted that his team’s option, developed at a public hospital, would be a lot cheaper. Commercial prices for this type of treatment are normally in the range of €300,000 ($338,000) per patient.
The ARI project is named after Ariana Benedé, an 18-year-old with acute lymphoblastic leukemia (ALL) whose case helped bolster research before her death in 2016. The team at Clínic Hospital developed another CAR-T treatment against that type of leukemia, which they named ARI-0001. In February, it became the first European CAR-T to be authorized by a regulatory agency. The price tag is under €90,000 ($102,000).
The Barcelona team’s new CAR-T treatment for multiple myeloma, presented on Friday of last week, has shown “spectacular” results, according to the director general of Clínic Hospital, Josep Maria Campistol. Besides a 60% rate of complete remission, 75% of patients showed no progression of the disease a full year later. Fernández de Larrea also noted that there was no evidence of neurotoxicity, which is a major concern with this type of therapy. Adverse immunological effects were also reported as mild.
The 30 individuals who participated in the trial had responded poorly to regular therapy against multiple myeloma. That is why Joan Gel insists that he would not be “here” if not for the hospital’s efforts to develop an alternative. “I want to underscore how lucky we are to have a public healthcare system of this caliber,” he said at the news conference. “We should be aware of that and pressure those with the ability to fund this healthcare and keep it in the front lines, where it should be.” Besides public funding, the project also received €5 million ($5.6 million) from the La Caixa Foundation.
The project has drawn praise from other cancer researchers in Spain. “The results are similar to other CAR-T [treatments] against multiple myeloma being developed by the pharmaceutical industry, with the difference that this is an academic and local development of therapies that are quite expensive and very complex,” said Joaquín Martínez, head of the hematological tumor research unit at Madrid’s 12 de Octubre hospital. “It has great merit.”
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
¿Tienes una suscripción de empresa? Accede aquí para contratar más cuentas.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.









































