The immense challenge of cancer vaccines: ‘There are promising results’
The consolidation of other immunotherapies and the rise of messenger RNA platforms have boosted scientists’ optimism. However, they point out that there won’t be a universal vaccine for cancer, but rather many highly-personalized ones


The dream of a cancer vaccine — capable of stimulating the immune system to fight tumors — is on the horizon of the scientific community. It probably has never been as close as it is now. After years of few successes in this field, the consolidation of other immunotherapies and the success of messenger RNA (or mRNA, which was used in the development of vaccines during the pandemic) have revived the optimism of scientists. The results have been promising, both in a recent trial looking at melanoma — with a vaccine prototype in combination with another immunotherapy — and in other preliminary research related to pancreatic cancer.
For years now, the success of vaccines when it comes to infectious diseases — the most recent case being Covid-19 — has driven multiple attempts to replicate these findings in a disease as devastating as cancer, which kills 10 million people in the world annually. But it’s not that simple. In ailments caused by viruses and bacteria, vaccines usually work preventively, exposing an individual to a weakened or inactive version of the microbe, so that their immune system learns to identify these threats and is able to neutralize them when they appear.
However, a tumor is much more complex and finding an effective vaccine can end up being an odyssey. Cancer is different in each patient, which forces scientists to design more personalized vaccines. And, unlike with viruses and bacteria — which our body knows to detect as foreign and harmful agents — cancer cells come from us. They look like our normal cells and have the ability to camouflage themselves and escape the body’s defensive army. Hence, a vaccine alone may not be enough.
Despite these differences, the idea behind cancer vaccines is to train the immune system to recognize cancer cells and eliminate them. To do this, tumor antigens (such as neoantigens) are used as a decoy. These molecules — which are found on the surface of tumor cells — are distinguishable from normal cells. Finding the most suitable antigens and administering them in the vaccine efficiently is key to triggering a good response from the immune system and making the vaccine successful. There are various approaches, from using vaccines based on DNA, mRNA (such as the Covid vaccines), peptides, dendritic cells, or even resorting to so-called oncolytic viruses, which are microorganisms capable of activating the immune system.
On paper, the proposal to awaken the body’s natural defenses to fight tumors is infallible. However, in practice, the triumphs of vaccines in cancer can be counted on the fingers of one hand. Among preventive approaches, the injection against the hepatitis B virus has helped prevent liver cancer, while immunization against the human papillomavirus has reduced the cervical tumors caused by this disease by 87% among those vaccinated. As for therapeutic vaccines — which are used to treat patients already suffering from cancer — there are only a couple of examples of relative success: one against prostate tumors and another (derived from a bacteria that causes tuberculosis) for bladder cancer. But both cases offered very limited benefits and are no longer utilized.
Why there are so few successes
The road has been tortuous. And, although a lot of attractive preclinical research has been developed in recent decades, the studies haven’t gone further “due to several barriers,” warns Laura Angelats, a researcher in the Translational Genomics and Targeted Therapies in Solid Tumors group at the Hospital Clinic Barcelona. The scientist refers to the diversity of solid tumors, which are very heterogeneous and present different antigens. She also points out the key role of the tumor environment: “The tumor cells aren’t alone, but they have immunosuppressive cells around them that make it difficult for the immune system to intervene.”
Miguel Ángel Perales — an expert in cancer immunotherapy and vaccines at Memorial Sloan Kettering in New York City — mentions the heterogeneity of the tumor itself. “Several vaccines studied were only directed against a very small part of the tumor. In many cases, only one or two cancer mutations are needed to resist the effect of the vaccine.”
In a recent interview with EL PAÍS, oncologist Chris Klebanoff — another researcher at Sloan Kettering — also pointed out that one of the great difficulties for the development of successful vaccines has been “the lack of precise knowledge [regarding] the correct antigens that should be included in the vaccine.” Furthermore, the oncologist adds, “many cancer patients are older, which means that their immune systems have aged over time. And there’s also the fact that treatments — such as chemotherapy and radiation — can severely damage the immune system. Therefore, we’re seeing patients who have older and more damaged immune systems.”
Hope for those with melanoma
Despite setbacks, research continues in search of preventive vaccines for high-risk groups — for example, patients suffering from Lynch syndrome, who are more likely to develop colon cancer — and, above all, therapeutic vaccines, whose resurgence in the last decade gives experts more confidence. There are hundreds of investigations underway that are looking at the potential of vaccines in multiple tumors, such as gliomas, glioblastoma, urothelial tumors, ovarian and cervical cancer, small intestine and colon cancer, among others.
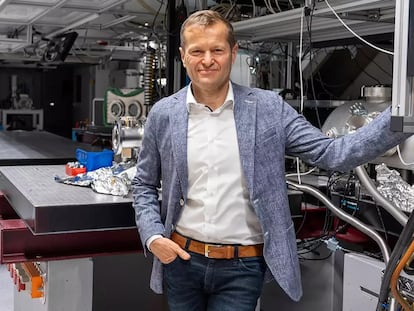
Peter D. Katsikis — a researcher in the Department of Immunology at Erasmus University Hospital in Rotterdam — has authored analyses on the challenges of developing personalized vaccines. Still, he emphasizes that the success of immunotherapy in recent years “has revived interest in vaccines against cancer. A vaccine against cancer neoantigens is expected to improve immunotherapy and perhaps expand its application to tumors that don’t respond to it.”
Some studies, in fact, have reopened the door to hope. “The results are promising,” affirms Luis Álvarez-Vallina, head of the Cancer Immunotherapy Clinical Research Unit at the Spanish National Cancer Research Center. The pharmaceutical companies Moderna and Merck, for example, are studying a prototype vaccine against melanoma that uses the mRNA platform. And, according to both companies, this preparation — in combination with pembrolizumab, a checkpoint inhibitor, which is a type of immunotherapy drug that helps deactivate the brakes that the tumor places on the immune system — has managed to reduce the risk of recurrence. Mortality rates were reduced by 44% in a phase II clinical trial. Phase III is already underway. “In a few years,” Álvarez-Vallina predicts, “we’ll have vaccines, while personalized vaccines could reach the clinic very soon.”
Current trials are focusing especially on the most immunogenic tumors — that is, those that are recognizable to the immune system and where immunotherapy usually works. The more neoantigens a tumor presents, the more immunogenic it will be. Melanoma is an example, but not the only one. “The tumors caused by tobacco — such as lung or bladder tumors — also generate many aberrant neoantigens. In these diseases, there are [phase I clinical studies] in which you increase the response time, by adding an autologous vaccine to the immunotherapy, made from the patient’s own tumor,” explains Josep Tabernero, director of the the Vall d’Hebron Institute of Oncology in Madrid.
Perales also highlights the “promising results in lung cancer” of a DNA vaccine. “It was shown that, one year after starting treatment, more patients in the vaccine group were still alive than those who had received chemotherapy.”
Combining vaccines and immunotherapies
Results have also begun to be seen in tumors in which — until now — other immunotherapies alone hadn’t achieved great success. A preliminary study in pancreatic cancer — one of the deadliest types of cancer — showed that a vaccine, in combination with a checkpoint inhibitor and chemotherapy, managed to activate the immune system in eight of the 16 patients in the trial. None of these eight patients had a relapse during the 18-month-long duration of the study.
There are many lines of research underway, but mRNA platforms are — according to experts — one of the most promising approaches. “The revolution [is in the form of] the new mRNA vaccines and the tools that allow us to enhance neoantigens and make vaccines on demand. If we manage to activate the immune system efficiently by using RNA platforms that allow us to generate vaccines with 24 neoantigens, we’ll achieve very important responses. This is the way forward,” says Álvarez-Vallina.
Scientists agree that cancer vaccines alone are not enough. The most encouraging results have been seen in therapies combined with other treatments. This joint approach can sometimes overcome the hostile tumor microenvironment that doesn’t allow the immune system to work. “Especially in solid tumors — in combination with checkpoint inhibitors — mRNA vaccines are going to mean an increase in [the number of] long-responding patients,” says Álvarez-Vallina.
Pending challenges and excessive optimism
Cancer vaccine research has stepped on the accelerator, but there are still some loose ends. For example, Álvarez-Vallina notes the troubles of “personalization, which involves logistical and budgetary complexity, and finding the appropriate combination of antigens that can be effective for a group of cancer patients.” The heterogeneity of tumors forces vaccines to be manufactured one by one, specifically for each patient, which implies a high cost. But solutions are still being sought.
“There are tumors that have common antigens and prepared vaccines can be made, for example, in [the case of] melanoma. But in other cancers — such as the pancreatic or colon cancer — the antigens are very varied. Studies are being generated to see what antigens 20% of patients have in common,” Tabernero explains. The oncologist — who warns of the complexity of these therapies and warns about “excessive optimism” — emphasizes that, when it comes to tumors, “the cells are heterogeneous and they evolve and the antigens disappear — the same ones that the tumors were made with.” This can subsequently influence the response to therapy.
When and to whom the vaccines will be administered are also questions that are on the table. “From the data we have today, we see that the most feasible application is in tumors in earlier stages, post-operation,” says Angelats, from the Hospital Clinic of Barcelona. Oncologist Chris Klebanoff is of a similar opinion: “Initially, it will be only for a subset of cancers, probably cancers where a surgeon has removed all of the observable disease. So, we are using the vaccine in an earlier disease setting, trying to prevent the recurrence or relapse of the cancer. That’s the most likely place where cancer vaccines might show an effect.”
It’s unclear how long a possible cancer vaccine would work for, whether its effect would be forever, or whether booster doses would be required. “We don’t know,” Angelats admits. She calls for caution and adds that, in any case, “the results obtained must be consolidated” in the first trials and “these treatments [must be tested] in other types of tumors other than melanoma.” Katsikis also sees “widespread implementation unlikely in the short-term.” Clearly, there are still chapters to be written in the promising story of cancer vaccines.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition