Cheap, quick and accessible: The cellphone Covid-19 tests currently under development
A number of scientific teams are developing new methods that can identify a coronavirus infection without the need for special equipment

To bring a pandemic under control, it is vital to know who is infectious – i.e. the people who have a sufficient viral load to infect others, whether or not they are showing symptoms. From the start of the coronavirus crisis, researchers have been working on developing domestic, portable and accessible measures to detect the potential of an individual to transmit the disease at any time. These technologies have now reached cellphones.
The team headed by the Spanish biotechnology expert César de la Fuente, at the University of Pennsylvania, has created three systems. Meanwhile, a team at the University of California has developed a model based on smartphones for SARS-CoV-2 and flu tests, without the need for special equipment.
De La Fuente, one of the best-known Spanish academics internationally and Presidential Assistant Professor at the University of Pennsylvania, has been warning since the start of the coronavirus crisis that “PCR tests are an excellent method for detecting an infection, but not necessarily for determining if the person is contagious.” In order to solve that shortcoming, he has developed a number of cheap, fast and efficient prototypes that detect the virus. The latest step has been to bring these systems to cellphones given their global, immediate and efficient qualities.
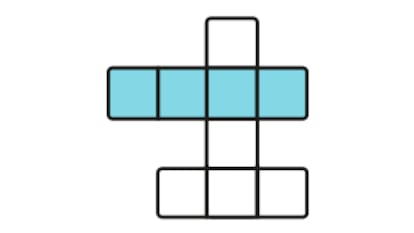
“We have developed a total of three prototypes for smartphones,” explains De la Fuente. “The first two use electrochemistry to detect the virus.” To do this, the team has created a chip upon which a fluid sample from the nose or mouth is placed. Via an electrochemical reaction, the S protein – the one that is used to infect – is used to determine whether or not the virus has managed to enter the cells of the organism using the AC2 receptor, which is the human cellular door via used by the coronavirus. These chips are connected to a laptop or smartphone via a potentiostat, which allows for the control of various variables in an electrochemical cell. All of the technology that the team is using has already been developed and is available. What’s more, the system has now been picked up by the science magazine Matter.
Colors of the infection
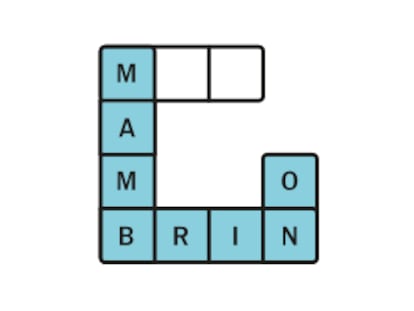
The third prototype, published in the scientific journal ACS Nano, relies on nanotechnology rather than electrochemistry. “It’s basically a cotton swab, like those used for the best-known tests, which is introduced into a liquid that changes color if we are infected,” explains De la Fuente. “It’s a colorimetric test, similar to a pregnancy test. A free cellphone application allows for the detection of the intensity of each pixel (the smallest element of an image) and that allows for the correlation of that qualitative image into something quantitative.” In this way, the cellphone identifies the viral load according to the color of the sample.
Each use of the first tests has an estimated cost of €4.15 ($4.73), while the second is as cheap as €0.15 ($0.17), and needs no more complimentary technology than a cellphone and the free app. The results take no longer than four minutes and are efficient with samples with high and low viral loads.
“The results,” the researcher explains, “are similar to those of a PCR or a conventional antigen test. We can detect miniscule quantities of the virus.” The team at the University of Pennsylvania is now in contact with companies that want to develop this technology and move to the production and sale phases.
De la Fuente’s team has been one of the first, but not the only, to advance in this field, which has been fundamental not just for the pandemic, but also for future infections with other pathogens, some of them as common as the flu, which can be diagnosed at home in a question of minutes and at a minimal cost.
Smartphones are very powerful tools to analyze biological assays such as clinical diagnostic testsAlexander Edwards, Associate Professor in Biomedical Technology at University of Reading
A team from the University of California has published another model in the Journal of the American Medical Association (JAMA). It has a sensitivity that is similar to the most-used tests until now, and, according to the main author of the study, Douglas M. Heithoff, has the capacity to be “easily modified to identify new variants of SARS-CoV-2 and other pathogens with pandemic potential, including the flu.”
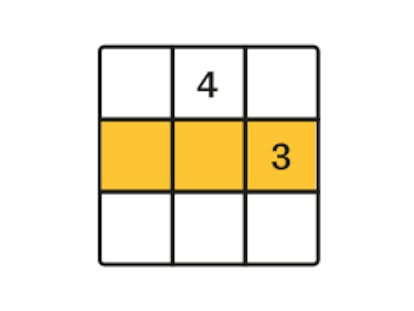
This last proposal makes use of loop-mediated isothermal amplification (LAMP). It’s a technique that amplifies DNA, costs little and is very common in molecular biology for the diagnosis of specific illnesses.
This detection system on smartphones based on saliva samples consists, according to the authors of the study, “a hot plate, cardboard box, and LED lights.” “The system is inexpensive to set up and portable; it can be fabricated for less than $100 [€88].”
These systems are key in a situation where the primary healthcare system is overwhelmed and a virus is highly contagious. They allow for the validation of the viral load in a fast and precise manner, among large amounts of people, and in particular in countries that have the fewest resources. Cheap and accessible self-testing is also key during a period when restrictions are being lifted.
Alexander Edwards, Associate Professor in Biomedical Technology at the University of Reading, asks the question: “Why the delay? Why aren’t all diagnostic tests operated by our smartphones, and instead are run on big machines in labs?”
Quoted on the website Science Media Center, Edwards explains that this research “adds to our confidence that we can detect important diseases like Covid-19 or influenza virus infections outside the lab. [...] The challenge remains how to deliver large scale product based on this type of technology, and to make simple, accessible products that people can make use of.
PCR tests are an excellent method for detecting an infection, but not necessarily for determining if the person is contagiousCésar de la Fuente, professor at the University of Pennsylvania
“Smartphones are very powerful tools to analyze biological assays such as clinical diagnostic tests,” he continues, “even just using their cameras without modification, because so many lab tests provide color-based or visual results.”
For Kevin McConway, emeritus professor of applied statistics at the Open University (United Kingdom), the work of the University of California has a limitation that the authors of the research themselves identify. “This study uses participants from a hospital setting in the US, and things could possibly turn out very differently in use in other settings in low- and middle-income countries where, they rightly say, it could be most useful.”
Equally cautious is Michael Head, a researcher from Southampton University (United Kingdom). However, he admits: “The use of mobile technology and remote health programs are likely to form a key part of how health systems operate in a post-pandemic environment. However, many of these approaches are still ‘the future’ rather than the here-and-now.”