How the United States embraced psychedelics
After half-a-century of prohibition, the United States is about to legalize psilocybin and MDMA for clinical use, to treat people suffering from post-traumatic stress disorder or terminal cancer. Scientists, patients, clandestine therapists and war veterans speak with EL PAÍS about the bright spots and shadows of this rebirth
Things were not going well for Marjorie Smith. The combination of a leukemia diagnosis and a divorce led to her depression. But Smith had read somewhere that the use of psilocybin — the active ingredient in hallucinogenic mushrooms — could help treat anxiety in patients with her condition. So, she told her oncologist: “If one of those trials is ever happening, count me in.”
When that day finally arrived, Marjorie put on a mask and headphones playing instrumental music. She took a high dose of the powerful psychedelic substance and lay down on a couch. After half-an-hour, she had a panic attack. She felt like she was in a “black box” that she wanted to get out of at all costs. The psychologist who was accompanying her and who had participated in her preparatory sessions managed to calm Marjorie down with breathing exercises. The patient lay down again… “and that’s where the adventure began,” she recalls.
“My ‘trip’ — very vivid — was divided into three chapters,” the 60-year-old woman notes, during a conversation with EL PAÍS in a downtown Washington cafe. ”One [part was] about my family, another was about my separation and the third was about being patient and tolerant.”
Obviously, the hallucinogens didn’t cure her leukemia — “this disease will be with me for [all the time] I have left” — but her treatment helped her return to being “her usual self… a positive woman.”
“It was wonderful,” she smiles. “I would do it again.” Still, due to the stigma that surrounds these substances, she prefers that her parents and coworkers not find out about the sessions. That’s why “Marjorie Smith” is a pseudonym, hiding yet another unexpected protagonist of the psychedelic drug boom in the United States. After half-a-century of prohibition, these substances are experiencing a second youth in a country plagued by an epidemic of mental health problems, fentanyl abuse and suicides.

The place where Smith tried the drug “for the first time” was at a clinic in the suburb of Rockville, Maryland, north of Washington, DC. Sunstone Therapies is on the third floor of the Aquilino Cancer Center, its affiliate institute. In 2020, it became the first non-university site to receive permission from the U.S. Food and Drug Administration (FDA) to conduct clinical trials with psilocybin, which is pending general approval for its expected medical use, either in 2024 or 2025. The conclusions of that first study with 30 patients — and without a placebo group — were published in the Journal of the American Medical Association (JAMA). These findings were encouraging: participants claimed that they felt less fearful about their conditions, while also managing to become more accepting about their fate.
One morning in July, oncologists Manish Agrawal and Paul Thambi opened the center’s doors to EL PAÍS. Both of them are the children of immigrants from India. Recently graduated, they met while working at the National Institutes of Health (NIH), before shifting into private practice. Treating patients suffering from “end-of-life stress,” they read a 2018 study which argued that psilocybin could offer cancer patients six months of relief from their existential anguish. This convinced them of the need to build a “healing center,” where they now also work with other psychedelic drugs, such as lysergic acid (LSD), MDMA — popularly known as ecstasy — or 5-Meo-DMT, the molecule behind ayahuasca. “We became very good at fighting tumors, but the quality of life of these people is something else… and we weren’t taking care of it,” Agrawal admits.
Sunstone Therapies’ facilities are clean and modern. Built at a cost of $1.2 million — much of which was raised from donors — it resembles a spa more than a clinic. There are four therapy rooms and a safe in which “the medicines” are kept. Patients don’t pay for the treatments, which cost thousands of dollars: this is also covered by donations. “When we did the first study, we were so moved by the response that we decided to do this,” Agrawal explains.
The center is named after 84-year-old psychologist Bill Richards, who also works there. A man with a broad smile, he was the last doctor who — back in 1976 — legally administered psychedelic drugs to cancer patients at the Maryland Psychiatric Research Center, before their use was prohibited by the authorities. The restrictions were collateral damage of the War on Drugs that was declared by President Richard Nixon in 1971. In an interview from his home in Baltimore, Richards recalls the “feeling of helplessness” at being deprived of a tool he considered to be beneficial for many patients. Before being banned, some 40,000 Americans took hallucinogenic substances in clinical settings in the 1950s and 1960s. Today, it’s estimated that more than 100 FDA-authorized clinical trials are underway to treat two dozen diseases.

Richards came into contact with psilocybin in 1963, while he was studying in Germany. He began working with it. “When the U.S. government offered me a scholarship to treat alcoholism with LSD, I returned. Then, those drugs hit the streets and Nixon declared Timothy Leary ‘the most dangerous man in America.’”
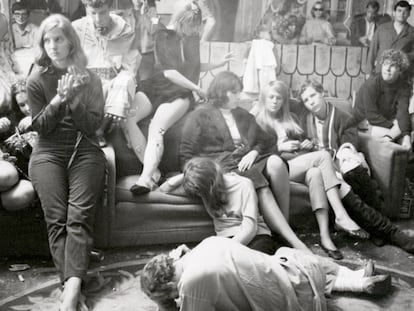
These were the years of the hippy explosion. Leary — a doctor in Psychology — had founded the Harvard Psilocybin Project with Richard Alpert in the early-1960s, to document the effects of this powerful natural entheogen on the brains of a handful of volunteers. Amid accusations of malpractice, the university closed the project. Banished from the academy, they transferred their proselytism to popular culture. Leary — who ended up becoming a fugitive from justice — coined a famous counterculture phrase: “Turn on, tune in, drop out.” He uttered this in 1967, the year of the Summer of Love, in front of some 25,000 hippies at a festival in San Francisco.
Whether he was a hero of the counterculture or a villain of psychedelic science, Leary’s rush to lead a revolution embodied the psychosis of the parents of a society undergoing a social transformation. The U.S. authorities encouraged misinformation about the ravages that these drugs could cause in children. And this is how, in the 1970s, psilocybin — which had been used for centuries in Mexico for ceremonial purposes — and LSD, a molecule accidentally synthesized in 1938 by Swiss chemist Albert Hofmann, ended up being classified along with dangerous substances such as heroin.
In reality, the probability of dying from an overdose after consuming LSD or psilocybin is extremely low. There’s also little chance of getting addicted to them, according to the DEA. Of course, when consumed by those suffering from certain physical and psychological conditions, these substances can lead to traumatic experiences, or manic or psychotic episodes.
Almost a quarter-of-a-century after its therapeutic use was banned, Richards was also there to witness its rebirth. In 2000, together with psychopharmacologist Roland Griffiths — from Johns Hopkins University, in Baltimore — he obtained the FDA’s authorization to carry out a clinical trial with psilocybin again. The pair’s results were published in 2006, in a scientific article about its potential to provoke mystical experiences. This is considered to have been the first step in the renaissance of psychedelic science taking place in the U.S. Despite the considerable cultural shocks, the FDA is set to approve the use of psilocybin in treating patients with mental health problems, as Australia already did on July 1, 2023.
Amidst this boom, the Center for Psychedelic and Consciousness Research at Johns Hopkins University continues to be a trailblazer. Hidden in a nondescript building on a campus east of Baltimore, researchers carry out research experiments on those suffering from addictions, severe depression, or anorexia, while treating patients with Lyme disease or Alzheimer’s. The center’s answering machine — which offers seemingly endless options — disabuses anyone of the notion that it’s easy to participate in a trial. Many people phone after reading an article like this or after watching a Netflix documentary.

The media seems obsessed with the subject of psychedelics. “If we said ‘yes’ to all the requests we get from reporters around the world, we would simply have to drop everything else,” jokes psychologist Albert García-Romeu, who has spent the past decade studying and treating addictions at the Baltimore center. “I think there’s a lot of trendiness in all this [interest], like when someone buys a Peloton or signs up for the latest diet,” he adds. “This is how the world we live in works: attention spans are very short. When [psilocybin] is approved for medical use, it will seem less sexy and, I hope, the waters will calm down.”
This trend that García-Romeu describes — together with the hope that psychedelic therapy offers — could mean the first psychopharmacological innovation of mass reach since the emergence of Prozac in the 1990s. In 2022 — according to official figures — about 1.4 million Americans will consume these substances for the first time, without medical supervision (27% more than in 2018). The figure is similar to the number of Americans who picked up smoking during the same period.
That same year, the publication of the largest psilocybin study to date — carried out by the British company Compass Pathways, which, along with the American Usona Industries, is the firm best-positioned to obtain FDA approval — revealed adverse effects (including suicidal thoughts) among some of the patients taking higher doses. This bolstered the arguments of those who criticize psychedelic therapy: they claim that medical professionals in favor of it are minimizing the associated risks, to prevent something from going wrong on its path to legalization.
There are several obstacles along this path, including the greed of the pharmaceutical industry (Compass Pathways has been criticized for trying to patent substances and practices that have been used for centuries). There’s also the concern that such treatments will be trivialized, given the massive market of wellness. There’s the possibility that the rosy conclusions of all the preliminary studies surrounding psychedelic drugs may be due to the researchers carefully selecting trial participants. And, of course, there’s the risk that — due to their high prices — even if these compounds are helpful, they will only be accessible to those who can afford good insurance.

If the 20 scientists consulted in this report agreed on something, it’s that these drugs “aren’t for everyone.” They warn that it’s essential to take them with medical guidance. These experts also emphasize that having too many expectations isn’t a good thing: many patients who seek these treatments hope for transformative experiences that don’t arise, leaving them disappointed.
For now, the FDA has published a draft protocol for medical trials. It aims to standardize criteria before these substances can be administered in private clinics. One such treatment that has emerged in recent years throughout the country is ketamine-assisted therapy, based on a substance that’s legal in the United States… although its reputation suffered a setback when it was recently associated with the death of Friends actor Matthew Perry. The FDA is aiming to bring some order to the increasing demand for psychedelic-based treatments and to prevent therapists (who have good intentions) from unintentionally harming patients. There are also discussions about setting limits on physical contact during sessions, to avoid cases of sexual abuse when a patient is incapacitated.
The death of a pioneer
Three weeks before EL PAÍS visited Baltimore, Roland Griffiths — the founder and director of the Center for Psychedelic and Consciousness Research — died at age 77 from colon cancer. After helping hundreds of people deal with end-of-life anxiety, he was able to apply his own methods to himself when he was diagnosed with the disease.
Neuroscientist Frederick Barrett succeeded him at the helm of the center. Dr. Barrett — who received his PhD with a thesis on the effects of music on the brain — excitedly explains his future plans: “We’ll leave behind the Elvis model — with a charismatic leader — to move on to another more orchestral one. [We will rely on] brilliant individuals from a group of world-class experts of different interests.” Barrett estimates that, in the almost 25 years that the center has been open, they’ve administered nearly a thousand doses of psilocybin — without incident — to more than 500 people. Each patient received between six and eight hours of prior therapy, in addition to the session itself, which lasts as long as the effects of the drug lasts (around six hours). There’s also a follow-up required, to take in what has been experienced. This final portion is what is known as “integration.”
“A deep connection is generated — in many cases, a very intimate one — with the patients,” explains psychedelic therapist Mary Cosimano. A legend in her field — and a strikingly empathetic woman — she spends the first five minutes of her interview with EL PAÍS in Baltimore asking about this reporter’s well—being and state of mind. She participated — along with Griffiths, Richards and Bob Jesse, another key name in the resurgence of psychedelia — in the trial at the beginning of this century that revived the medical use of hallucinogens. “We had to keep it a secret; we couldn’t talk about the experiment with our families. We had to prevent [the information] from spreading… something like that would have been fatal [for the project],” the therapist recalls.

The ritual that she has participated in so many times — the silent room, the mask, the headphones — is more or less the same as in the 1960s, when Richards helped put together a musical playlist dominated by classical composers such as Brahms or Vivaldi. Although it has been updated, the playlist is still in use. “We believed in the need to have two therapists — a man and a woman — because of the representation of the maternal and paternal figures… and also because someone had to turn the record around,” Richards clarifies. Streaming has solved the requirement of flipping the vinyl’s face, while two therapists aren’t always present anymore (labor is what makes these therapies so expensive). Still, the process is designed to avoid bad experiences based on taking care of two basic concepts: the set and the setting.
A conference in Denver
Last June, the Psychedelic Science 2023 (PS’23) conference was held in Denver, Colorado, a state that has taken the step (along with Oregon) to decriminalize the possession of hallucinogenic mushrooms. It was proof that the set and the setting are fit for the comeback of psychedelic therapy in the United States.
The event was organized by MAPS — a non-profit organization that stands for the Multidisciplinary Association for Psychedelic Studies. It was founded in 1986 by Rick Doblin, a charismatic guy with a single mission in life: to achieve the legalization of MDMA for the treatment of patients with post-traumatic stress disorder, including victims of sexual violence or war veterans.
Ecstasy is a synthetic drug, which was introduced into psychiatric practice in the late-1970s by the chemist Alexander Shulgin, who is credited with being the author of some 320 psychoactive compounds. Molly — as it is popularly known in the United States, where it was legal until 1985 (and for a brief period two years later) — also jumped from the laboratory and took over nightclubs, becoming a part of rave culture. The authorities ended up making it illegal for medical use.
One of the two branches of MAPS is a pharmaceutical company that was recently renamed Lycos. It has raised over $100 million from investors and has completed the third and final phase of clinical trials. It is now approaching FDA authorization, which could arrive as soon as this year or next.

The event in Denver — which brought together some 12,000 participants (for $900 a ticket) in a convention center that hosted 477 talks on 11 stages — was opened by Doblin, with a presentation in which he launched a provocative slogan: “Net-zero trauma by 2070.” In a later interview, he explained that he’s not afraid to “err on the side of optimism.”
“Humanity is in crisis and I’m convinced that psychedelics can help it significantly,” he added.
The heart of the event was a scientific conference in which the conclusions of clinical trials — carried out by dozens of universities throughout the country and also by foreign entities, such as the Imperial College of London — were presented. There were lectures focused on the reform of drug policy and the opportunities available to the pharmaceutical industry, a business that moved around $40 billion in the United States in 2022. Some speakers discussed the effects of microdoses of hallucinogenic substances, whose method — taking imperceptible quantities on alternate days, between 5% and 10% of a full dose — was popularized by another octogenarian pioneer, the psychologist James Fadiman. He began this after learning that Hoffmann — the inventor of LSD — had practiced it for decades.
In a Zoom call from San Francisco, Fadiman explained that, since 2011, he has been documenting stories of people who have managed to reduce their anxiety and depression — or increase their concentration and creative abilities — via microdosing. However, there’s currently no consensus within the scientific community regarding these conclusions, for two reasons: because it’s difficult to separate the effects experienced by patients who actually consume the substances versus those who take placebos. Generally, when people expect to benefit from medication, they usually do. “Placebo is a manifestation of the body’s natural ability to heal itself. So, if microdosing doesn’t actually do anything and you heal yourself... what’s wrong with that?” Fadiman shrugged.
Another major focus of the Denver convention was directed at the PTSD experienced by several veterans — a fundamental piece in the puzzle of the psychedelic rebirth. Stories like that of Amber Capone — the wife of a retired military man — has convinced various Republican politicians — such as former Texas Governor Rick Perry, who participated in the conference — to support the legalization of psychedelics in heavily conservative states, so as to ease the return of soldiers to society.

Marcus Capone belonged to the elite Navy Seals for 13 years. He was deployed seven times to Afghanistan and Iraq. Upon being discharged, his depression, anxiety, alcoholism and irascibility devastated his family life. “It became an existential struggle,” his wife Amber notes in an interview with EL PAÍS. When they concluded that psychiatric treatments and antidepressants weren’t solving the problem, they decided — as a last resort — to try ibogaine in Mexico. This is a plant of African origin that takes the consumer on a demanding mental loop of about 12 hours. “He came out of there a new man. He didn’t want anything to do with alcohol. It was miraculous,” she gushes. The couple then decided to found an association to help others in their situation.
Amber Capone didn’t seem like your typical psychedelic drug meeting attendee, but Denver really had everything. The battered psychonauts mixed with newcomers eager for knowledge, as well as a wide range of experts. There were undercover FBI agents, politicians, academics, therapists and so-called “underground practitioners,” who have been offering these treatments outside the law for decades.
The attention that these substances are receiving and the rigor in the criteria for participating in a clinical trial have made the guild of psychedelic counselors grow exponentially. Their clients often look to them not because they’re experiencing a mental health issue but because they’re seeking to have a significant — even transcendental — experience. Those who have worked with these substances long before clinical trials at universities were an option have earned the respect of scientists. “They’ve been accumulating enormous knowledge through private practice for decades… That knowledge should be used when these drugs are legalized,” Mary Cosimano, of the Johns Hopkins Center for Psychedelic and Consciousness Research, affirms. On the other hand, for those who are new and inexperienced — and, in the worst cases, attracted by the trendiness of psychedelic drugs or the potential profits — it’s more problematic for scientists to put their hands in the fire for them.
It took a couple of months for EL PAÍS to find someone who wanted to tell their story without hiding their name. Jahan Khamsehzadeh finally waived anonymity and spoke with us from Oakland via video call. He notes that he has held “about 500 [psychedelic] ceremonies” and that he walks “the line that separates the surface (where he publishes books and participates in podcasts) and the underground.” After all, he’s dedicated to something that’s currently illegal.
“I’ve studied a lot. I don’t feel like I’m doing anything wrong, and I think the feds don’t come after you unless you make a lot of money, or if you sell drugs. Since I started this [practice], I feel more confident with each passing week, because science supports us,” he affirms. Khamsehzadeh — who charges “between $2,000 and $3,000 a session” — works with cocktails of substances that the FDA is unlikely to approve, although he believes that he’s prepared to be totally above-board “when the time comes.”

Fadiman says that, in the past, he collaborated with the DEA. An official made it clear to him that there was no benefit in pursuing the clandestine business of psychedelics. “‘Why?’ I asked him. ‘There’s no money there,’ he told me.”
Rahul Gupta — the White House’s drug czar — confirmed in an interview in Washington that the priority of the Biden administration — which has decreed the forgiveness of all minor federal convictions for marijuana — is quite different. Amidst the fentanyl crisis — the largest drug crisis in the country’s history — Gupta’s commitment is to treat addicts “like patients” and to avoid filling prisons with those who have broken drug possession laws.
In How to Change Your Mind — the book that has done the most to spread the resurgence of this phenomenon — essayist Michael Polland turned to clandestine practitioners to tell the story of the failure of the first wave of psychedelia and about the ongoing second wave. In a conversation in Denver, Pollan noted his concern about the proliferation of “unscrupulous underground therapists who take advantage of people.” Regarding his role in the movement, he said that — when he published his book in 2018 — he couldn’t guess how much he was contributing to the renaissance. “Something was about to change in [the culture]... I was just lucky enough to [predict it] before the pandemic hit and we all started looking for help,” he explained. “We must also take into account our proverbial enthusiasm: when we Americans see a train passing, we take it to the last station.”
The writer spoke on the main stage of the conference, reserved for politicians, rockers (Melissa Etheridge), Hollywood actors (Willow Smith), podcast stars (Andrew Huberman) and other big names. As big as that of American football star Aaron Rodgers, who recalled his “coming out” as a psychedelic user, when he recounted that he had participated in an ayahuasca ceremony. Rodgers — who, in 2022, brought the hallucinogenic concoction to homes across the country when he celebrated a touchdown by forming a circle with his teammates and pretending to drink the concoction from imaginary bowls — argued that this experience had helped him improve his performance. “The year before [ayahuasca], I had 26 touchdowns, four interceptions. A good season,” he explains. “[I took] Ayahuasca… 48 touchdowns, five interceptions, best player in the league. What do you say to that?” After his signing by the New York Jets, the quarterback’s past season — plagued by injuries — has been rather forgettable.
The conference — perhaps because it was held in the West — also had the electricity typical of fortune seekers during the Gold Rush. Especially in the part of the fair with 300 exhibitions, where venture capitalists prowled. There were start-ups, laboratories that presented patents for new substances, psychedelic law firms, luxury travel agencies to facilitate the consumption of substances in Jamaica and Costa Rica, as well as companies selling kits to grow mushrooms at home. Against this backdrop, ethnopharmacologist Dennis McKenna — whose legend dates back to the trips he made to the Amazon in the early 1970s with his brother Terence, a legendary psychonaut — lamented: “Unfortunately, psychedelics don’t cure the disease of capitalism.”
McKenna also warned of another of the contradictions of this second boom: “Much of all this is borrowed from Indigenous communities. There’s a long and shameful history of looting their drugs. The white man arrives, takes the plants, synthesizes them and becomes a millionaire.” At the conference, concerns about the representation of Indigenous peoples were constant. There was also criticism of the extractive dynamic that’s affecting the consumption of ayahuasca in the Amazon jungle, or the sale of peyote, a cactus that grows in the deserts on the border between the United States and Mexico. During the closing speech, Doblin — the advocate for MDMA — was interrupted by a group of protestors.
While it wasn’t possible to interview Doblin during the conference, EL PAÍS tracked him down a couple of months later. He spoke to this newspaper from his home in Boston on video call. “They’re expressing themselves from a position of deep pain that has been inflicted on them for centuries, but that was a scientific conference. We’ve learned from Indigenous peoples, but also from modern scientists. I think that, if we waited for those Indigenous leaders to organize a congress like that, it would never have been held. And, by the way, MDMA doesn’t come from any plant.”

A career psychologist, Doblin — who experimented with LSD in the 1970s — decided to dedicate his life to ecstasy because “it’s the kindest of psychedelics.”
“I’m not dedicated to science, but to political science,” he clarifies. “[MDMA] is a substance with great potential to help people and it’s the easiest to sell in society. Who can deny help to combat trauma?” He also clarifies that, when the FDA gives it the green light, it can be prescribed for other purposes under what is known in the United States as “off-label.” This is what happens with medicines when they’re used for purposes other than the original one. “The nuance is that the insurance companies won’t cover it in those cases,” he clarifies.
Here’s an important nuance: a dose of MDMA can be found on the street for a handful of dollars. But if it’s part of therapy within a savagely capitalistic healthcare system (like the American one), it can cost up to $11,000 when prescribed. “I don’t like that,” Doblin says, “but we also have to take into account the millions that we’ve invested in achieving FDA approval. This has forced us to look for investors… investors who want profits,” he warns. “All in all, the amount isn’t that high if you compare it to the expenditure of years of psychotherapy.”
The same thing happens with psilocybin (and its comparison to the cost of chemotherapy). Again, what makes the final bill more expensive is the labor of the sessions before, during and after taking the substance. To complete the picture, we must mention the criticism levied against the pharmaceutical company Compass Pathways, whose representatives preferred to skip the Denver conference to avoid protests. “They tried to patent a production process and even the ritual of the sessions, which would have forced others to pay them for working with psilocybin. A lot of people didn’t like that,” according to Doblin.
Another challenge has to do with scale. If these treatments are legalized, it will be more difficult to control who administers them and how, but also who receives them. A recurring warning invites us to take into account that the funnel with which volunteers are currently selected is very narrow. The patients who are taken for the trials are carefully chosen — something that will be more difficult to maintain when the treatments are opened up.
There’s also curiosity to know how the great religions plan to react to substances that have been used for centuries as a source of generating mystical experiences. Following the 2006 Supreme Court ruling in favor of freedom of worship for a sect (in its desire to import ayahuasca for use as a sacrament), “psychedelic churches” have proliferated in the United States, with permission to celebrate such ceremonies. Given this scenario, Pollan asks: “Will Islam or Christianity see these substances as a threat to their authority? Will they banish them from [houses of worship], or incorporate them into their spiritual practices?” The answer could lie in the conclusions of a study that will soon be published. It was carried out by Johns Hopkins and NYU with religious leaders who have received high doses of psilocybin.
In all these questions, there’s an effort by the psychedelic community to prevent the train from derailing. It won’t be easy, according to drug policy reform activist Adam Smith, who’s often associated with a famous 1980s slogan, “The war on drugs is a war on us.” This phrase — which he insists came out of a collective creative process — points out that decades of prohibition have disproportionately impacted minorities. “The legalization of marijuana (allowed in 38 of the 50 states for medical use and in 24 for recreational use) is a good example that there are many ways to do [drug policy incorrectly]. We must closely follow the first mushroom decriminalization experiments in Oregon and Colorado and learn from our mistakes,” he warns.
Psychologist Bill Richards — perhaps because he has already witnessed the death and resurrection of psychedelic science — isn’t so worried. “These substances,” he recalls, “have been in use since more or less the 5th century BC. They emerge in the culture, they’re suppressed, and they re-emerge. Today, the pendulum is returning them to the [mainstream], but the best we can hope for is to educate the masses to use them responsibly. If things go wrong later, at least we’ll have tried.”
For now, the United States certainly seems ready to try again.
Sign up for our weekly newsletter to get more English-language news coverage from EL PAÍS USA Edition
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.