What epidemiologists have learned about the coronavirus 18 months into the pandemic
More than 600 public health specialists met this week in Spain to discuss everything we now know about Covid-19. Here are their main findings


During the first years of the HIV/AIDS epidemic, those who caught the virus, suffered and eventually died had no idea how they had contracted it; diagnosis was a death sentence. Those years were a time of fear and stigma. Fast forward to the current Covid-19 pandemic, and scientists had identified the virus before the disease even had a name, or before the vast majority of the population had even heard of it.
What we see today is a reflection of the progress of science in the four decades that separate these two devastating pandemics. A few months of 2020 passed “using a sledgehammer to crack nuts” in the words of Fernando Simón, the epidemiologist who serves as Spain’s Director of the Coordination Centre for Health Alerts and Emergencies. And while there is still much to learn, many fundamentals about the virus are already known.
Simón referred to this progress at the annual meeting of the Spanish Society of Epidemiology (SEE), held last week in person in the city of León. After a year and a half of video calls, many specialists were able to see familiar (masked) faces, and tried to identify other colleagues and journalists they had only talked to via screens. This is one of the lessons learned since March 11, 2020, the day the World Health Organization (WHO) classified Covid-19 as a pandemic: although social contact spreads the virus, it can be safe if certain measures are taken. The following are some of the lessons that epidemiologists shared at the meeting.
In-person meetings are safe (under certain circumstances)
The first thing that the society’s president Elena Vanessa Martínez had requested was that this meeting be held face-to-face. “We have discovered that many things can be done remotely, but sharing knowledge and experiences at a meeting like this is much richer in person,” she said. With case numbers falling and practically all the attendees vaccinated, a rigorous safety protocol was also applied: limited capacity in the lecture rooms, at least two seats separating the attendees, adequate ventilation, hand gel and masks. “There was a digital contingency plan in case the numbers were too high, but it wasn’t necessary,” said Martínez. The president of the organizing committee, Tania Fernández Villa, explained that the measures were based on those that were already successful at the University of León, where classes were mostly held face-to-face, as they were in Spanish schools. Spain was the only country in Europe and one of a few in the world to keep physical attendance close to 100% without a big spike in the number of cases in the classroom.

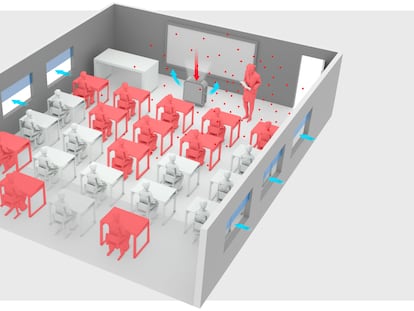
The virus is in the air
Probably the biggest paradigm shift since the beginning of the pandemic was our understanding of how the coronavirus is transmitted. At first, it was believed that infection occurred through small droplets of saliva left on surfaces. An infected person could leave droplets behind that if touched by an uninfected individual could enter the body through their eyes, nose or mouth. “Not a single infection like that has been demonstrated,” said José Luis Jiménez, one of the researchers who insisted early on that the virus could be transmitted through the air. Today we balk at the images of supermarkets in the earliest lockdown days, where people can be seen walking around wearing gloves but no masks. The SEE president believes we should insist on more caution where “it is known that the virus is most transmitted,” like enclosed places where people go to eat and drink, removing their masks to do so.
Lockdown was useful for stopping the virus
The spring 2020 lockdown across much of the globe was a very drastic measure, but it did reduce the transmission of a virus that was then fairly unknown and circulating in an uncontrolled way. Although lockdowns clearly reduce infection rates, they are blunt instruments that can also damage society and the economy. As the months went by in Spain, regional health authorities also resorted to closing internal borders within the country to limit domestic travel, and the usefulness of that is now less clear.
Micro-lockdowns
Adrián Hugo Aginagalde explained that some anti-Covid measures were applied with “very limited” evidence and that evaluating them posed “enormous difficulties”. “Some of the restrictions that affect mobility do not always obtain the expected result. There have been apparently successful experiences and others where it has been very difficult to measure,” he said. One example was Madrid’s micro-lockdowns of specific neighborhoods, or even streets, based on their proximity to a given healthcare center. One study found that this measure had no impact on virus transmission at all. Another produced mixed results, with a fall in transmission in areas with very high rates of infection, but little change in areas with slightly lower rates when the restriction was imposed. Carlos Fernández, the author of one of these studies, said he believed these micro-lockdowns were “of very limited” use. One of the problems, Aginagalde argued, is that in places where people are required and allowed to leave their homes for work, their workplaces may be the places they are getting infected in the first place. There is also no evidence that sealing off the borders between regions, as was done for months in Spain, had any useful effect.
Masks are useful to stop infection, but how useful?
It is very difficult to quantify how masks stop the virus from infecting wearers. There are so many factors that influence physical behavior that it is practically impossible to isolate each one. One of the largest studies to date (still preliminary), conducted with hundreds of thousands of people in Bangladesh, showed that in populations where the use of face masks increased, the risk of infection dropped from 8.6% to 7.6%. But the research is very limited: it did not evaluate whether masks were worn correctly, and it did not have a control group of non-mask wearers. Only symptomatic cases were counted. Among older people, the infection risk fell by 34.7% compared to 9.3% in the general population, probably because more cases were detected because there were more obvious symptoms. It is known that masks are useful, but it is very difficult to say by how much.
Age is the greatest risk factor
One of the conclusions that became clear very early on is that older people are the most vulnerable after contracting Covid-19. Age correlates most closely with the risk of dying from coronavirus, but a closer look at the data shows that the problem seems to be more closely linked to frailty (although very often they go hand in hand). In people over 65 years old, the risk of dying is four times higher (40% of those infected) among people with severe frailty than in people whose health is considered robust, according to a preliminary study carried out in Catalonia and presented at the SEE conference.

Risk of infection is linked to socioeconomic factors
If the risk of death from Covid is determined by age, the link between risk of infection and socioeconomic factors “has not been sufficiently studied,” according to Carmen Vives, a professor of public health at the University of Alicante. People who need to leave home in order to work, those who live in overcrowded conditions, and those in more vulnerable situations are much more at risk than their wealthier counterparts. Another preliminary study, also carried out in Catalonia, showed that the richer a nursing home was, the lower the risk of death for its residents. Epidemiologists have known for decades that one’s postal code has a greater influence on health than their genes. That’s still true for Covid.
Public health systems need to be improved
Spanish epidemiologists were unanimous that public health systems need to be improved. Manuel Franco, spokesperson for the Spanish Society of Public Health (Sespas), despaired at how public hospitals were overwhelmed. “They have not increased staffing levels, and technology has not been sufficiently improved. We have had the biggest healthcare crisis in a century and we don’t see any money being invested in this. It’s hard to believe,” he said.
Miguel Hernán, a professor of epidemiology at Harvard University, opened the event by reviewing the strengths and shortcomings of Spain during the pandemic. One of the negative points he raised was the lack of a large public health agency, which the government has promised to set up. “That’s the model of other countries like Germany or the United States, which have an institution led by respected scientists and independently providing recommendations to politicians. These are the decision-makers, but if they don’t follow [the experts’] advice they have to explain why.” In Hernán’s opinion, Spain is very proficient at data collection, but it is incapable of implementing a system that uses it, gives it value and converts it into recommendations for politicians.
We have to keep learning
In August 2020, a group of Spanish experts called for an independent review of the management of the pandemic in a critical letter to the scientific journal The Lancet, among them Helena Legido. At the conference, Legido sat at a roundtable with Fernando Simón, the head of the government’s health emergencies department, where she continued to defend the need to evaluate everything that has happened so far in order to make better decisions in the future. “Despite all the lessons we had learned in previous health crises, the world was not prepared to face this one. And in Spain we lack a critical culture of evaluation. It already happened to me when I studied the impact of austerity measures; it is very difficult to get those in power to listen and react,” she said. Simón pointed out the difficulty of stepping back to evaluate what has been a relentless crisis. “Those of us who know best what has happened have been working non-stop to deal with the pandemic,” he defended.
Without an independent, rigorous assessment, however, it will be difficult to take measures to mitigate the effects of a future pandemic. And one day it will come.
Tu suscripción se está usando en otro dispositivo
¿Quieres añadir otro usuario a tu suscripción?
Si continúas leyendo en este dispositivo, no se podrá leer en el otro.
FlechaTu suscripción se está usando en otro dispositivo y solo puedes acceder a EL PAÍS desde un dispositivo a la vez.
Si quieres compartir tu cuenta, cambia tu suscripción a la modalidad Premium, así podrás añadir otro usuario. Cada uno accederá con su propia cuenta de email, lo que os permitirá personalizar vuestra experiencia en EL PAÍS.
En el caso de no saber quién está usando tu cuenta, te recomendamos cambiar tu contraseña aquí.
Si decides continuar compartiendo tu cuenta, este mensaje se mostrará en tu dispositivo y en el de la otra persona que está usando tu cuenta de forma indefinida, afectando a tu experiencia de lectura. Puedes consultar aquí los términos y condiciones de la suscripción digital.