Spanish hospital workers on frontline of coronavirus crisis: “This is the war of our generation”
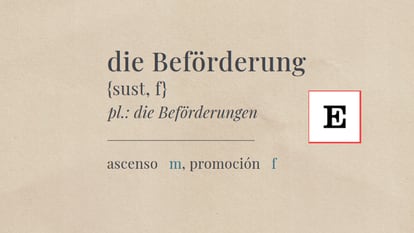
Staff at Intensive Care Units across the country talk to EL PAÍS about the pressures and challenges they face when trying to save patients suffering from Covid-19
/cloudfront-eu-central-1.images.arcpublishing.com/prisa/QQHHZKRJEVC2ZHJCBZT6I4HZOA.jpg)
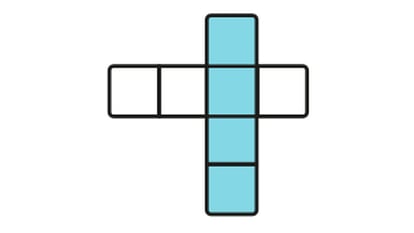
“I’ve never experienced anything like it. The ICU [Intensive Care Unit] is a very intensive job, but now we are overwhelmed, you can’t even leave to pee,” says a doctor at the Getafe hospital in the Madrid region, which has been hardest hit by the coronavirus outbreak. Intensive Care Units have become filled with seriously ill patients, some sedated, others intubated. All are hooked up to various tubes. They are alone, in some cases until their death. All have the same diagnosis: Covid-19, the disease caused by the SARS-CoV-2 virus.
The hospital wards face a seemingly unstoppable avalanche of patients. On Sunday, 173 more people were placed in intensive care in Spain, bringing the total to 1,785. More than 700 are in wards in Madrid, which has doubled its capacity.
A swarm of hospital workers, dressed in medical gowns, caps and double gloves, rush to help the ill. There are thousands of health workers, with typically one nurse for every two patients. Their faces are marked by fatigue and anguish. They have never faced such an enemy – one that is very contagious and still unknown – nor such a distant horizon. The patients in their care take a long time to recover, remaining on average two to three weeks. This is the experience of the people running and working in Spain’s life-saving Intensive Care Units.
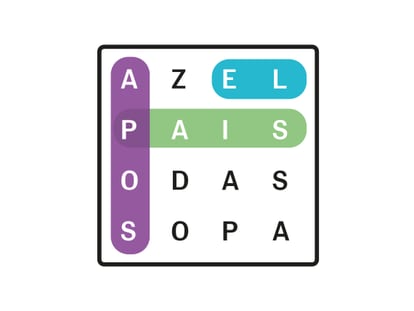
“You can’t breathe”
“The work is immense, draining, stressful. You are in a gown, with a face mask and cap, you can’t breathe and your glasses fog up. I have never experienced anything like it. It’s titanic. I wish it were a film that I could watch the end of,” says María Antonia Estecha, 57, the head of service at the ICU at the Virgen de la Victoria Hospital in Málaga, in southern Spain. For the past two weeks, she has been working with patients in a critical condition while trying to avoid contracting the virus, all with the knowledge that the worst is still to come.
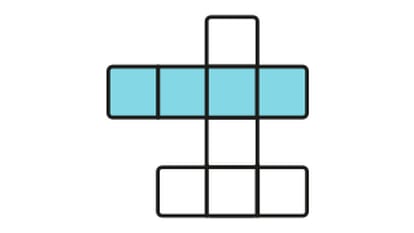
An ICU, with its specialist beds and severely ill patients, is always an intense workplace. But now more so than ever: “Everyone has the same pathology: serious pneumonia that requires emergency intubation and connection to a ventilator,” says Gabriel Heras, an intensivist at a hospital in Madrid. “It requires a lot of time and human resources and experts. Also, it’s been shown that sick people respond very well to oxygenation when they are faced down. Four or five people are needed to do this for a sedated, intubated patient. Sixteen hours are indicated. We put them face down at 3am and we turn them over at 7am.”
This technique, particular to this crisis, is doubly delicate. It could take half an hour, says Estecha, and require the help of nurses, guards and support staff. “The doctor is at the head of the patient because if the tube falls out you die,” she explains. What’s more, there is a greater risk of spreading contagion through the air.
“The situation is terrible. We are swamped and subjected to a very high level. The fear of being infected is constant,” says a nurse at the ICU in La Paz hospital in Madrid, which is one of the health centers under the greatest strain.
The fear of being infected is constantNurse at the ICU in La Paz hospital in Madrid
“They are not doing the tests that they should. They are facing sick people with a very high viral load. They are very worried about the lack of protective gear,” says Guadalupe Fontán, from the Spanish Nurses Association.
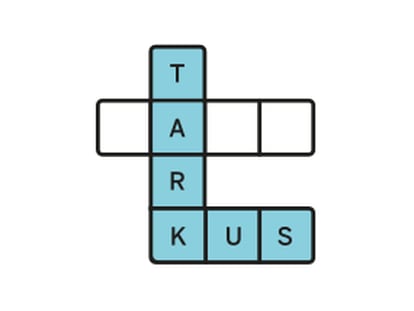
“The ICUs were working with open doors, with families,” says Fontán. “That can’t happen now. So we ask families to send audio messages and we give them to [patients] to listen to.”
The anguish of seeing someone dying completely alone on your shift. The fear of getting infected and infecting your loved ones. Seeing the shortage in medical equipment. All of this weighs heavily upon you, say the emergency workers. Agustín Vázquez, a nurse at the Gregorio Marañón hospital, stands in front of a closed door. On the other side are the isolated patients. He doesn’t remember there being such silence since the terrorist attack on the Atocha train station in Madrid on March 11, 2014. And he knows the silence is going to last.
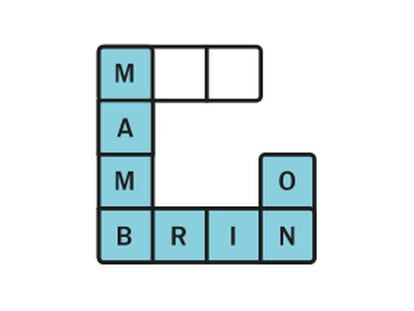
It takes five minutes to put on all the protective gear needed to enter the ICU. “First we put on gloves, then the gown, the face mask, the cap, the protective glasses, like the ones used for skiing, a visor like those used by riot police. Then another set of gloves,” says Vázquez.
“Working with two sets of gloves requires a tremendous amount of effort. Imagine catheterizing a vein like this. There is always someone outside keeping watch in case we get dizzy. You have to give a warning when you want to leave, and then we do the reverse process of getting undressed. Every time we take something off, we have to clean ourselves with alcohol gel. And we do this in pairs so that we that nothing fails.”

Despite his fatigue after finishing the night shift, Vázquez has simple demands: “We don’t have enough resources, high-efficiency face masks, visors and impermeable disposable gowns. We need more protective glasses. Now we are disinfecting them and we reuse them.”
The hospital workers on the frontline of Spain’s coronavirus crisis want equipment, weapons for a war whose battlefield can change within hours. “We are in a kind of war dynamic,” says a young nurse at the Princesa hospital in Madrid. “We organize jobs so that we only have to enter a patient’s room at most two or three times per shift, to reduce the risks and so we don’t have to use so much gear.”
“I decided to become a doctor after the terrorist attack at Atocha station,” says Celia González, an anesthetist at the Cruces Hospital in Bilbao, in the northern Basque Country. “This is the war of our generation.”
Fear of shortages
Workers in intensive care units are concerned about how a shortage of resources could affect patient treatment.
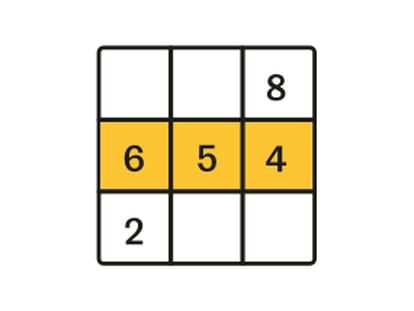
“You give every patient the support they need,” says Ricard Ferrer, the head of the ICU at Vall d’Hebron hospital in Madrid. The problem, he says, is that intubation is not suitable for elderly patients. “It’s so invasive that if you apply this technique you wouldn’t be able to remove it. People who are more fragile are given high-flow nasal cannulas which provide warm and humidified oxygen to the body.”
Gabriel Heras, an intensivist at a hospital in Madrid, warns that a shortage of equipment could force doctors to make difficult decisions. “I read that Italian professionals are saying they are not going to attend to patients over 65, which sounds awful,” he says. “But if you only have one respirator, and you have to choose, we have to prioritize people with the greatest chance of survival. We haven’t reached that point yet, but we could get there and it will be very painful. The system is not going to be able to take in all the cases that are coming in.”
English version by Melissa Kitson.
/cloudfront-eu-central-1.images.arcpublishing.com/prisa/TJNITS475ZEGTFZAOIJE7FAAPE.JPG)
/cloudfront-eu-central-1.images.arcpublishing.com/prisa/R4EBAXV52NHSRBHNNRKTACFEQU.jpg)