Spanish health authorities crack down on opioid abuse
Studies have detected excessive prescriptions of immediate-release fentanyl, a drug 100 times more powerful than morphine


The unjustified prescription and abuse of immediate-release fentanyl, a potent opioid, has put the Spanish authorities on alert.
The Health Ministry and Spain’s regional governments have decided to establish a working group “to evaluate and improve the use of opioids, particularly when delivered in forms that pose a greater risk of addiction,” said sources who participated in the latest Interterritorial Council, which adopted the decision.
The move follows the publication of data on opioid consumption by the Spanish Medicine Agency (Aemps) indicating a 79% increase between 2010 and 2017. Some experts note this is simply due to fentanyl being used more widely for legitimate medical purposes.
If it’s on the increase, it’s because pain is being treated more and better
Mª Angeles Canos, La Fe Hospital
“If it’s on the increase, it’s because pain is being treated more often and in a better way,” says María Ángeles Canos, head of the Pain Unit at La Fe Hospital in Valencia. “There’s no reason to stigmatize a family of very useful drugs that significantly improve patients’ quality of life.”
However, authorities have detected sporadic cases of unjustified prescriptions of immediate-release fentanyl, which is dispensed through inhalers or dissolved in the mouth, acting against pain more quickly than slow-release patches.
This drug is up to 100 times stronger than morphine and is considered the most potent opioid on the market. It is also highly addictive and should only be prescribed in very particular circumstances, namely to cancer patients suffering from breakthrough pain, says Antonio Alcántara, secretary of the pain unit of the Spanish Society for Primary Healthcare Workers (Semergen). Breakthrough pain is sudden and temporary onslaught of intense pain.
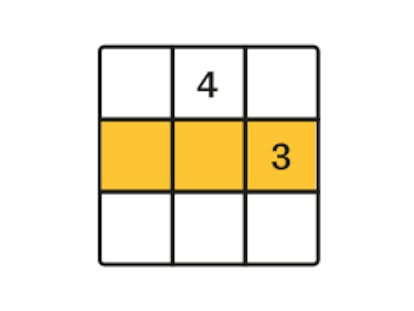
Patient pact
Be familiar with the patient's background. The guidelines for chronic pain relief for non-cancer cases conclude that the most reliable indication of inappropriate use of opioids is a prior history of abuse.
Health records. As the source of information on drug and prescribed drug abuse is the patient, a complete case history and regular check-ups are the best way to detect possible abuse.
Digital prescriptions. These provide a record of medicines prescribed for the patient in both the private and public sector.
Informed consent. This is a pact with the patient agreeing that if the treatment is not followed correctly, the prescription will be stopped and the patient sent to rehabilitation.
“That excludes non-cancer patients who have a greater life expectancy, and whose chronic pain must be treated with slow-release patches,” he says. “The use of immediate-release fentanyl should be restricted to the treatment of those suffering breakthrough pain.”
But specialists and the authorities are aware that immediate-release fentanyl is occasionally being too loosely prescribed. The Valencia regional government conducted a study in 2016 in which “we saw an increase in use which did not match the diagnosis and exceeded the recommended dosage or treatment period,” says Raquel Tena, deputy director general of pharmaceutical products at the Valencia health department. Following this investigation, 1,518 treatments were reviewed.
C.R.B. is 43 and admits to being addicted to PecFent, one of the commercial brands of immediate-release fentanyl. “Every day of my life, I curse the day I first tried it,” he says. His back problems started with a herniated disc, which was operated on in 2000. A year later, a traffic accident displaced one of the implanted screws. “You can see that I was used to living with pain, but it got much worse in 2015. The attacks were increasingly frequent and intense, and not only in the lower back region but also in the cervical area.”
C.R.B., who is weaning himself off the drug and prefers to remain anonymous, then started what he calls a pilgrimage from doctor to doctor in both the public and private sectors in search of a solution. “In the end, you get into what people like me call the quest for El Dorado: the route that will get you a prescription of anything that will relieve the pain,” he says. He first encountered opioids with tramadol. Then he moved on to subcutaneous morphine injections. After that, it was slow-release patches of fentanyl, and finally he moved on to the inhalers. “I hit bottom four months ago,” he says. “The people around me and my doctor all told me that this was the end of the line.”
Every day of my life, I curse the day I first tried it
C.R.B., fentanyl addict
Experts say that between one and five percent of patients show signs of risk. “But it is far from all patients who become addicted or dependent,” says María Ángeles Canos. “It is important to get to know the patient and find out if they have a history of dependency. They need close supervision and they need to be on board to help identify and respond to risky behavior.”
Both Canos and Alcántara agree it is important to establish guidelines for the management of opioids, which should be followed by all professionals.
But while there may have been an alarming increase in the use of highly addictive opioids in Spain, it is still a long way from the levels of abuse that exist in the US. The Aemps data also shows that most consumption is in drugs with a lower opioid content.
“In recent years we have moved from opioid-phobia to opioid-philia and probably it would be best to be somewhere in between,” says Alcántara, adding that he welcomes the move by authorities to more closely police prescriptions. “It will help to develop and distribute the use of guidelines that will avoid unnecessary risk.”
English version by Heather Galloway.