Instructions for dying
Fewer than one percent of Spaniards have made a living will Lack of information and a refusal to contemplate death keep numbers low


An ischemic stroke left Margarita bedridden. She was 78 and never woke up again. Her son Carlos says his mother, a small and frail woman, always wanted to "go" in a natural way.
"My father had died of cancer five years earlier and the last months of his life were a tremendous, useless period of agony in a hospital. She did not want that for herself," he explains.
And she left it in writing. Margarita did not want probes or life-prolonging treatment if her condition became terminal. And it was. Her children knew about the living will, and her doctors were informed. Margarita died under sedation soon later. "And she left in peace," says her son Carlos.
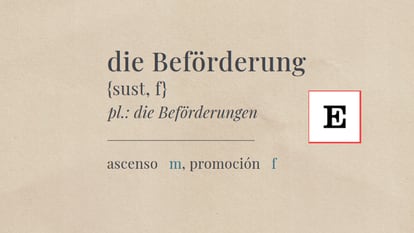
Like Margarita, around 150,000 people in Spain have made a living will with instructions - revocable at any time - on what type of healthcare they would like to receive in the event they become unable to express their wishes personally. It includes directives on cardiopulmonary resuscitation, the use of feeding tubes, organ donation and more.
Many health professionals are unaware of the living will system
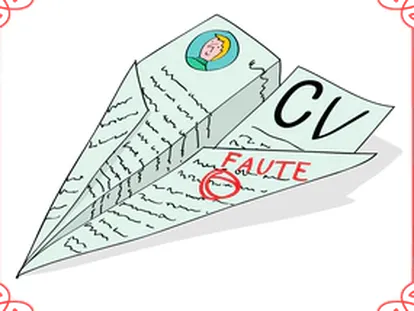
Twelve years after the Patient Autonomy Law regulated the expression of advance healthcare directives, the use of this right has yet to gain traction in Spanish society. A living will remains something of an unknown concept to most people, and even to health professionals, experts note. Adding to this barrier is the silence surrounding all things death-related in Spain, a country reticent to talking about the end of life.
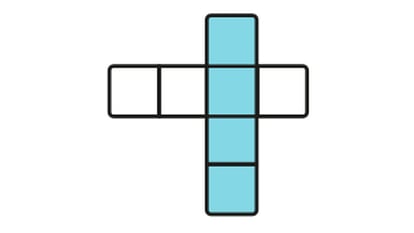
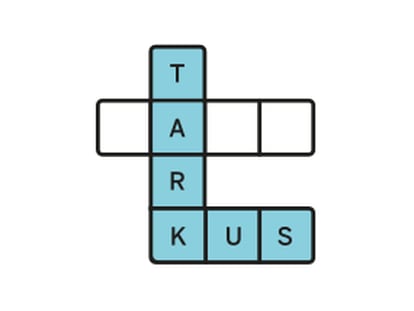
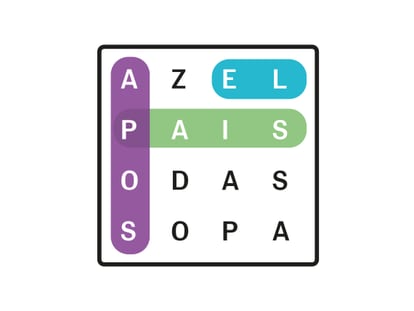
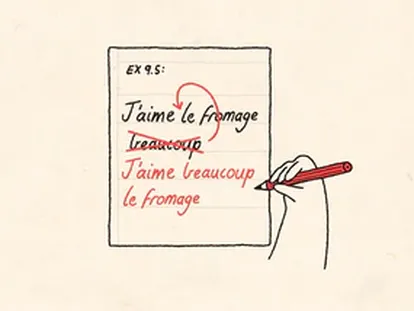
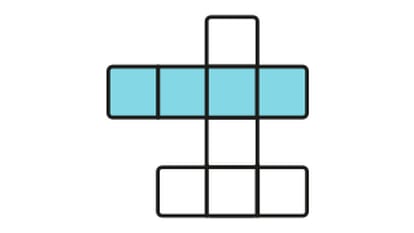
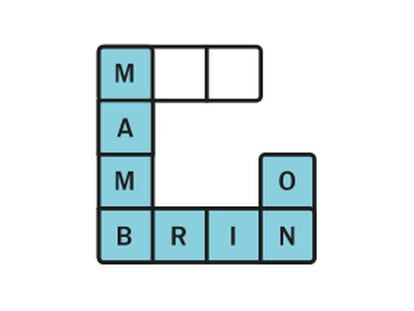
Anyone of legal age can make a living will or model one after existing documents drafted by regional governments, dignified death advocate groups such as Derecho a Morir Dignamente (the Right to die with dignity), or even the Catholic Church. The document is then either entrusted to a notary and signed before three witnesses with no ties to the will taker - all three must keep a copy - or else handed to the appropriate registrar's office in the regional government.
Since a few weeks ago, and for the first time ever, all regional records are connected to the National Living Will Register. If the need should arise, doctors can consult a patient's living will regardless of where it was drawn up and officialized.
Despite this, a significant amount of health professionals are unaware of the system, says Ana María Marcos, a professor of philosophy of law at the distance university UNED and chief researcher in a project about living wills.
The problem definitely exists, admits Juan José Rodríguez Sendín, president of the doctors' association Organización Médica Colegial. Sendín criticizes the lack of strategy to encourage use of the document.
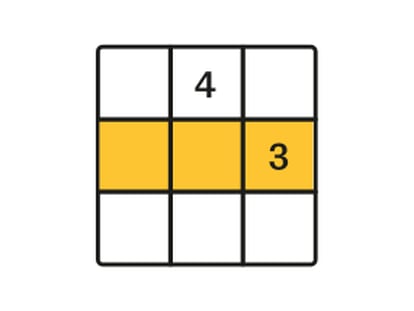
How to do it
- Anyone of legal age can register a living will. In some regions, such as Andalusia, minors who have left home can also create one. In Aragon, anyone over 14 is permitted to draw up such a document.
- There are several different models available - those drafted by regional governments and those produced by associations such as Derecho a Morir Dignamente.
- A living will document includes directives on which treatments the person would want and which they wouldn't in the event that they become unable to express their wishes.
- The living will needs to be signed in front of two or three witnesses who are not related to the person either by blood or by marriage.
"Hospitals have a code to consult whether patients have a living will. But not everyone knows about it," explains Marcos.
As a matter of fact, says Fernando Marín, president of the Madrid-based association Derecho a Morir Dignamente, few health workers review the system. Still others reject the entire concept of a living will.
"They feel that, being health professionals, they are the ones best placed to make decisions at that moment," says Pablo Simón, of the Andalusian Public Health School.
This is what happened to Antonio, a 76-year-old man who died of cancer a month ago after a brief but painful hospital stay, says his friend Federico.
"Even though we showed them his living will specifying that he wanted no external life-prolonging measures or painful procedures, the doctors insisted that he undergo tests that caused him suffering," he says. "It's as though their opinion ruled over our life."
It is not hard to find physicians who equate this tool for preventing therapeutic cruelty with euthanasia, explains Fernando Marín, of the dignified death association. It is the kind of confusion that could be solved with the right amount of information, but there is a great shortage of information in the Spanish health system, he contends.
Still, some steps are being taken to ensure health workers are aware of whether their patients have made a living will or not. In regions such as the Basque Country, there is a mention of it in a patient's electronic medical record. Now, the health ministry is analyzing the legal conditions that would enable authorized professionals to access a person's living will via a link on his or her medical record, according to a report that this newspaper has had access to.
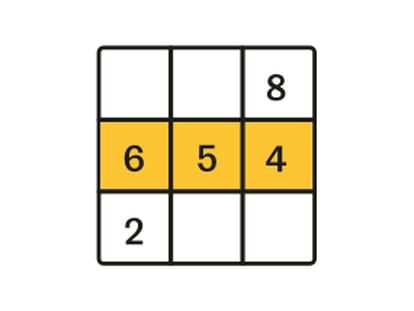
But fewer than one percent of Spaniards have made out a living will, compared with nine percent in Germany, for instance. There are also significant gaps between the regions: Catalonia and Andalusia have the largest amount of advance health directives on record, while Murcia, Ceuta and Melilla have a grand total of two. Women are a majority across Spain, according to ministry figures. It is as though women were more willing to think about the moment of death, or to talk about it - a rare thing in Spain.
"A living will is informed advance consent, a set of written instructions on what I want done to me and what I don't want done to me at a time when I am never going to be conscious again," says Marcos. It is this anticipation and the refusal to think about the end of our life that is keeping numbers low.
"Spanish culture is reticent to talk about death - either one's own death or the death of others. It's considered gruesome," says Pablo Simón.
Besides that, the context in which end-of-life decisions are made in Spain are very family-oriented. People figure that their own relatives will make the best decisions when they are sick. Although the point of the living will, notes Fernando Marín, is to clarify and facilitate this decision-making.
Experts say the best way to deal with this issue is for people to talk about their wishes with their doctors and families. In Spain, even though people increasingly want to have control over the process of death, there is still a long way to go before it can be talked about naturally.